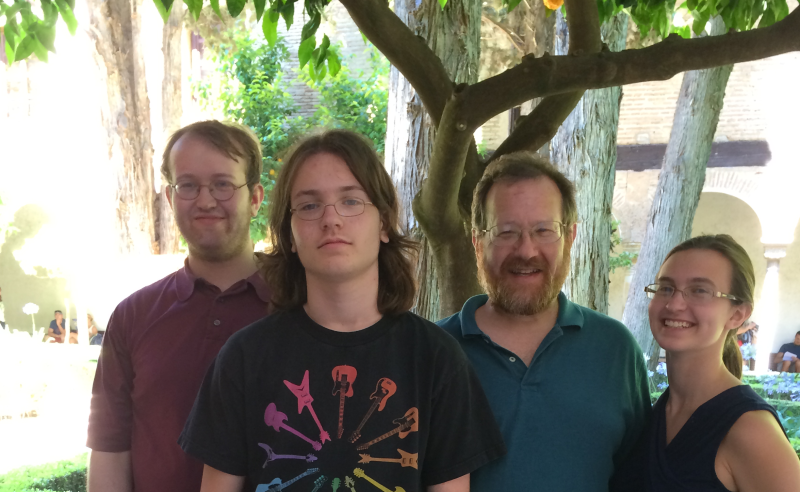
For this week’s faculty spotlight, we talk to David Edelman, MD, (pictured with his three children Adam, Isaac, and Sara, during a recent trip to the Alhambra in southern Spain), a 21-year veteran of the division of General Internal Medicine. In this interview, Edelman talks about health systems interventions to improve chronic diseases, why successful interventions for veterans and other specific populations don’t always translate to the general public, and his efforts to expand his cooking repertoire.
What are your responsibilities within the division? What does a typical day for you look like?
I’m Associate Professor and Fellowship Director for the Division. I teach a course in the Clinical Research Training Program (CRTP) in the fall, and I co-chair the Durham VAMC Institutional Review Board (IRB). I also direct a medical student fellowship that allows Duke Medical Students to get a funded Master’s degree, and I conduct research. Finally, I see primary care patients at the Durham VAMC one half day a week and precept residents in their primary care clinic one half day a week.
Because of this diversity, I don’t have typical days. Other than Wednesdays, which are clinical, the only thing that I am certain to be doing on any given day is sitting in my Legacy Tower office trying to clear emails.
Your current work involves preventing cardiovascular disease through health system interventions. Can you tell me more about this work? What kind of interventions in this area have you focused on? How do these efforts tie into interventions to improve patients’ health-related behaviors?
I’ve been doing randomized clinical trials of health systems redesign interventions for almost 15 years. Sometimes these interventions exist primarily to change the system in order to provide more focus on a particular clinical problem or set of clinical problems; sometimes they exist primarily to help patients adopt for healthful behaviors; sometimes there’s some of both going on. I’ve used group interventions, which often fall into the “both” category, in most of these studies; we had great success in a VA randomized trial of group medical clinics for diabetes and hypertension (we improved BP, reduced ER visits, and reduced hospital costs in the second year after the intervention).
That said, my latest trial assesses a group intervention for prevention of cardiovascular disease that is heavily oriented to changing patient behavior rather than health system focus. The intervention is informed by both motivational interviewing and problem-solving therapy (although the intervention is not truly psychotherapeutic) and attempts to get patients to overcome “internal” barriers to adopting healthful behaviors (that is, asking, “what is it about me that I don’t exercise, given that I know it’s healthy?” rather than “can you help me find the nearest place where I can swim?”). This is also a VA study.
You were the lead author of a recent study in the Journal of General Internal Medicine that examined telephonic nurse case management for patients with diabetes and hypertension. Can you tell me more about this study and how it came about?
Our VA group has had a fair bit of success with having nurses call patients and see if they can motivate them to change their behaviors. However, it seemed to me that this kind of work was fairly easy to do in the VA; it’s a vertically integrated system with a single electronic health record, and with academic providers who often want to improve the VA health care system. Duke Primary Care is a much more complex healthcare environment; it’s fee for service, the providers are very very busy, and it’s harder to integrate patients’ care that you give in a study into the flow of their regular primary care. So we designed a study to see if what had worked in the VA would work as well in Duke Primary Care.
Ultimately, the telephonic case management examined in this research did not lead to improved outcomes. What lessons can be drawn from this findings for future research and improving care?
The answer to the above question, for a number of really interesting reasons relating to both DPC and the individual study, was a resounding “NO.” From a research perspective the lessons we learned were: it is probably best to enroll subjects that are out of control in the key outcomes of the trial; and sample sizes for real-world trials should be larger than you think, both because sample standard deviations are unpredictable and because interventions lose potency when placed in a real-world context. From a clinical perspective we became the 4th study of the year 2014 to suggest that nurse telephone calls to influence behavior management are ineffective in real-world settings. This has now become an emerging literature suggesting that higher-potency interventions are needed in the real world than are often used in traditional randomized controlled trials.
Have you recently read any books, articles, blog posts or other material that would be of interest to the division?
I haven’t read anything lately that interests ME. I’m really hard to get excited… my answers to the above questions explain that, because so much of what we thing is “THE ANSWER” or even “an ANSWER” turns out not to work when you really do it.
What passions or hobbies do you have outside of the division?
I spend a lot of time with my family, much of that doing functional things like shopping and laundry, because life is busy. I do a lot of cooking lately; I can’t say I’ll be on “The Next Iron Chef” any time soon, but I have a dozen or so things I do well enough to serve to people that aren’t my family, and I’m trying to expand that repertoire. And I’m passionate about baseball; I just got back from an annual weekend with old friends where we go to a couple of major league baseball games and play a round of terrible golf (golf is NOT a passion or hobby of mine).