From the Director

The holiday weekend threw me off … so med res news is a bit late! If you are new here, expect this typically on Mondays (and even in the morning if I am on my game). But happy 4th, and happy new academic year to all!
Thanks to Lynsey, Madi, Jen and Tia who were incredible in getting our orientation put together and run smoothly! Also to Megan Gillum, Sarah Nouri and AJ Blood for organizing an all-GME last night of intern year get together for our now JARs. Much thanks to Dr. Kuhn for sponsoring as well! And a huge thanks also to our Stead leaders – with fearless Eileen Maziarz at the helm – for planning the night at Ponysaurus. Great representation from all.
Kudos this week to Dan Maselli, Maggie Moses, Meg Steiner, Jackie Bolwell, Ankeet Bhatt, AJ Blood, Kevin Smith and Shai Posner for putting together the intern boot camp this year. You did a great job – the first days of the year have gone really well, and it has been fun to see everyone in their new roles. Alyson and I walked around on Friday and every team was teaching like crazy.
The chiefs will be planning class get-togethers coming up, so be on the lookout for an email from Madi to let you know the details .
Please plan on attending grand rounds Friday … Jenn Rymer will be finishing out the 2015-16 Chief Grand Rounds! It’s in Trent Siemans, so plan ahead!
This week’s pubmed from the program goes to Anubha Agarwal, Adva Eisenberg and Dr. Sue Woods for their JAMA case “A Common Cause of Cranial Nerve VI Palsy Hidden in Plain Sight”. A second pubmed to Paul St Romain for the case he submitted to Global Morning Report!
Have a great week
Aimee
What Did I Read This Week?
Alicia Clark, MD
http://www.nejm.org/doi/pdf/10.1056/NEJMcp1514257
I read “Upper Gastrointestinal Bleeding due to a Peptic Ulcer” by Loren Laine from the “Clinical Practice” series in NEJM. I wanted to discuss this article for a few reasons. First, I love the NEJM “clinical practice” series for it’s content, design and clinical vignette approach. It is one of the first places I look when I am searching for a concise review and expert opinion on the approach to a common problem. It provides a great source for references to evidence based guidelines whenever they are available. I also appreciate this series because the writer will describe areas where there isn’t data to guide clinical decision-making and offers one expert clinical opinion. The second reason I chose this article is because we see Upper GI bleeding from ulcers so often. Finally, I am trying to incorporate high value care decision making whenever possible and this article brought up a few areas where I think we have some opportunity for improvement.
The case describes an otherwise well 55 y/o F on aspirin 81mg who presents with frank hematemesis and VS concerning with HR >100 and SBP <100. Initial labs show a hgb of 11 and normal platelets/INR. The author reminds us that an initial hgb is a very poor indicator of the severity of upper GIB, it takes hours and volume expansion to equilibrate. The tachycardia and hypotension suggest that she is lost 25-30% of her total blood volume and resuscitation should follow vital sign response. The article goes on to offer many clinical pearls about common etiologies for UGIB, diagnosis and treatment for H Pylori, high risk features and timing of endoscopy. It describes the Glasgow-Blatchford score which is a risk assessment tool that can help to determine who might be well enough to proceed to outpatient management and avoid admission (clearly not the patient in the vignette). It also references some of the extensive evidence behind employing a restrictive transfusion strategy (hgb goal >7) for pts who are hemodynamically stable.
As physicians, I think we tend to search for evidence to support our interventions but it is just as important to learn the evidence that supports when less intervention yields similar or better outcomes. Admissions to the hospital and blood transfusions are not without risk and both come at a cost. It is essential to consider the potential harms as well as potential benefits whenever considering an intervention.
One of my personal soapboxes is the potential overuse of protonix infusions. The author specifically addresses this issue by referencing the current guidelines that recommend bolus and continuous infusion of PPI for pts with bleeding ulcers and high risk endoscopic features. He then references the newer JAMA Meta-Analysis and systematic review in 2014 where “intermittent oral or intravenous proton-pump inhibitor therapy resulted in outcomes that were noninferior to those after continuous infusion”. In the summary, he describes dosing of PPIs for pts with high risk endoscopic features is an area that requires further study. However, I think we are safe to avoid the continuous infusion for pts with low risk endoscopy features (or maybe low risk GI bleeding in general?). When thinking about the “value” of an intervention, we have to consider potential harms and benefits. The harm of a continuous infusion PPI is not just cost in dollars but harm defined by the patient experience. Imagine your elderly patient being tied to an IV pole for 72 hrs and getting the sedating meds necessary for endoscopy. These kinds of tethers can worsen delirium which is associated with higher morbidity and mortality.
I hope this has at least given you reason to check out the clinical practice series in NEJM. See you on the wards!
Clinic Corner

Hi all!
Happy New Year! Welcome New Interns!
The 2016 Thrive Guide/ or Everything you need to know at DOC is here!
Thanks to the amazing hard work of Caroline Sloan, Sara Nouri and Megan Gillam!
They re-did almost all of it and reorganized it all!
Even if you are not new to DOC review it! There are many great details that I didn’t even remember!
And welcome to new DOC attendings, Greg Brown, Kathy Waite, Aparna, and in the fall Nia Mitchell!
Our new space at DOC almost ready to use, check out that huge room on the way to the break room….precepting in there, new desks, paint, carpet,
Looks awesome!
Likely precepting to start there by the end of July..stay tuned!
Lynn and Co.
Lynn Bowlby MD FACP
Medical Director Duke Outpatient Clinic (DOC)
Associate Professor of Medicine
Duke University SOM
Pager 919-970-4559
From the Chief Residents
Grand Rounds
Friday, July 8 - Jennifer Rymer, Chief Resident, DUMC, 2015-16 (held in Trent Semans)
Noon Conference
| Date | Topic | Lecturer | Time | Vendor | |
| 7/4/16 |
Holiday |
|
12:00 | ||
| 7/5/16 |
Welcome |
Chiefs | 12:00 | Mediterra | |
| 7/6/16 |
SAR Lecture Series: Chest Pain/ACS |
Zach Wegermann | 12:00 | Cosmic | |
| 7/7/16 |
SAR Lecture Series: Rapid Response Team Scenarios |
Andrew Demaio | 12:00 | Domino's | |
| 7/8/16 |
Chair's Conference |
Meg Steiner | 12:00 | Subway |
From the Residency Office
Have You Logged Your Duty Hours??
With the start of the 2016-17 academic year, the residency program is asking all house staff to log their duty hours on a daily basis. This will allow us even closer oversight of duty hour compliance across the program. In order to use the MedHub mobile Duty Hour app, you will need to know your actual MedHub log in as it will not accept your NetID/password log in. If you have forgotten you main log in, please go to the main MedHub site, and select "Forgot my password." You will then be able to re-set it via email. Lynsey Michnowicz will be sending reminders each Wednesday to those who have not yet logged their duty hours for the week. Thank you in advance for your attention to this task!
NCSP Applications
The National Clinician Scholars Program (NCSP), a two-year research training fellowship (formerly known as the Robert Wood Johnson Foundation Clinical Scholars Program) for physicians and nurses, is now accepting applications for enrollment in July 2017. The NCSP provides mentored training in clinical, community, and health policy research, with a focus on supporting the development of change agents who will devote their careers to leading improvements in health and healthcare.
The NCSP, in partnership with the Department of Veterans Affairs, currently has training sites at the University of California at Los Angeles, University of Michigan, University of Pennsylvania, and Yale University.
Applications are due August 15th.
Office Hours for Dr. Zaas
Dr. Zaas will have the following office hours. Please feel free to stop by during these times and of course always feel free to reach out to her office to set up a meeting outside of these times if needed!
Monday - 3:00 p.m. to 4:00 p.m.
Thursday 10:00 a.m. to 11:00 a.m.
LiveSafe Mobile App
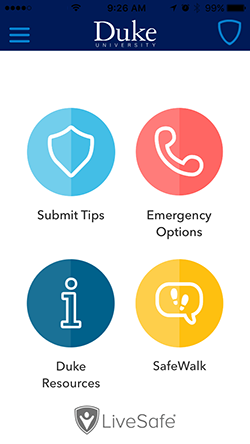
Duke is introducing a new mobile app called LiveSafe to put a powerful safety tool in the hands of the Duke community.
The app, available as a free download from Apple and Android app stores, enables smartphone users to submit real-time tips to Duke Police, virtually “SafeWalk” friends and family while traveling, place emergency calls, and access important resources for support.
You can find more information, including instructions on how to download the free app, on the DukeALERT website: http://emergency.duke.edu/notified/livesafe.
Opportunities for Wellness
Feeling down? Need to talk to someone?
All trainees at Duke have FREE access to Personal Assistance Services (PAS), which is the faculty/employee assistance program of Duke University. The staff of licensed professionals offer confidential assessment, short-term counseling, and referrals to help resolve a range of personal, work, and family problems. PAS services are available free of charge to Duke faculty and staff, and their immediate family members. An appointment to meet with a PAS counselor may be arranged by calling the PAS office at 919-416-1PAS (919-416-1727), Monday through Friday between 8:00 A.M. and 5:00 P.M. For assistance after hours, residents and fellows can call the Blood and Body Fluid Hotline (115 inside DUH, 919-684-1115 outside) for referral to behavioral health resources. Another resource is Duke Outpatient Psychiatry Referrals at (919) 684-0100 or 1-888-ASK-DUKE.
https://www.hr.duke.edu/pas/
Upcoming Dates and Events
July 29 - Summer Celebration @ The Home of Dr. Zaas
August 31 - Stead Trivia Night
October 8 - Stead Tread
Useful links
GME Mistreatment Reporting Site
https://intranet.dm.duke.edu/influenza/SitePages/Home.aspx
http://duke.exitcareoncall.com/
Main Internal Medicine Residency website
Main Curriculum website
Department of Medicine
Confidential Comment Line Note: ALL submissions are strictly confidential unless you chose to complete the optional section requesting a response
Opportunities
https://www.phs.wakehealth.edu/public/edu.cfm
www.bidmc.org/CentersandDepartments/Departments/BIDHC
http://www.careermd.com/employers/latestbulletins.aspx