
On January 6, 2020, the American College of Emergency Physicians announced that Duke Regional Hospital has received Geriatrics Emergency Department Accreditation (GEDA), which recognizes emergency departments that use protocols designed to meet the needs of older patients.
“This accreditation reaffirms our commitment to providing the very best care for older adults,” says Katie Galbraith, MBA, FACHE, president of Duke Regional Hospital. “I am so proud of our Emergency Department and Geriatric care teams who keep geriatric-specific initiatives top-of-mind in our busy Emergency Department.”
The geriatric-friendly strategies used in the Duke Regional ED range from the straightforward—keeping walkers, snacks, and water on hand—to the more involved, such as an interdisciplinary protocol for hip-fracture patients that provides fast, non-opioid pain management and a quicker transition to the operating room for those who need surgery. Taken together, these strategies reduce complications such as falls and hospital-acquired delirium.
The GEDA accreditation is one of many geriatric innovations underway at Duke Regional.
Galbraith says Duke Regional is perfectly positioned for focusing on the needs of older patients.
“As a community hospital, we are very much a part of this community and well respected by older adults—many of them have been coming to this hospital since we opened,” she says. “We are a little smaller and more nimble, and our team members get really excited about being able to try new things.”
Heidi White, MD, professor of medicine (Geriatrics), points out that Duke Regional is a comforting environment for older patients, with its smaller size, more intimate culture, and stress-free parking. Geriatric innovations that work at Duke Regional are shared with other Duke Health hospitals.
“We want older adults to experience the same quality of care no matter where they touch our healthcare system,” White says.
Victoria Orto, DNP, RN, NEA-BC, chief nursing and patient care services officer at Duke Regional, is always on the lookout for ideas to improve the experiences of older patients. That’s why she started Optimizing the Care of Older Adults, an interprofessional group that meets monthly at Duke Regional.
“I saw that our older adults had some clinical needs that weren’t being met consistently,” says Orto, “and in order to address that you need to have an interdisciplinary forum.”
The group includes physicians (from geriatrics, medicine, surgery, emergency department), nurses, respiratory therapists, physical therapists, occupational therapists, speech pathologists, care managers, pharmacists, as well as patient and family volunteers from the community.
“It’s one of my favorite meetings because everyone is so passionate and excited,” Orto says. “We all want to give great care to our older adults.”
Innovations
Two simple yet impactful innovations that have come out of this group are the Yellow Box and the Care Square.
The Yellow Box is a brightly colored cardboard box that hospital patients use in their rooms to stash glasses or hearing aids at night. Wearing glasses and hearing aids in the hospital is an important strategy to help older patients stay engaged and avoid delirium, but sometimes patients send these items home to avoid losing them.
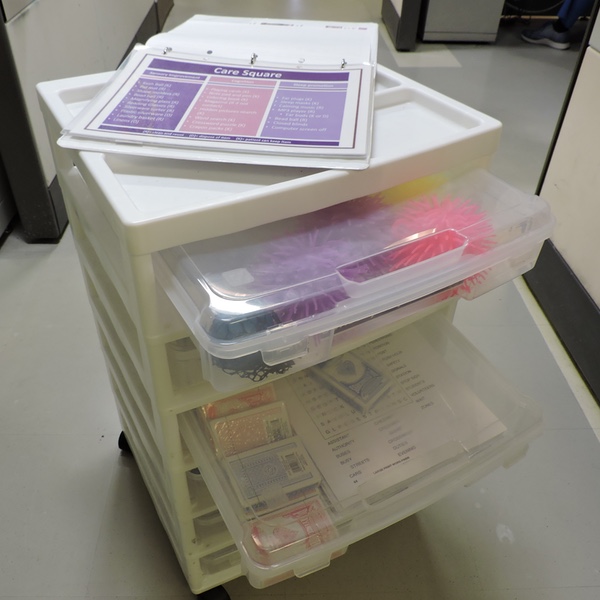
The Care Square is a “therapeutic activity cart” that aims to keep patients with dementia engaged and to help prevent delirium. The cart is stocked with cards, puzzles, music, and other items that provide sensory enhancement, cognitive stimulation, or sleep promotion. Like the Yellow Box, the Care Square was piloted at Duke Regional and is now set to be implemented at Duke University Hospital and Duke Raleigh Hospital.
The group also participates in larger projects, including the system-wide Mobility Redesign, which is being piloted at Duke Regional. It’s intended to ensure that older adults stay as active as practical while hospitalized rather than spending all their time in bed. Part of the redesign includes discouraging physicians from writing orders for bed rest unless absolutely necessary and having nurses do a bedside mobility assessment. Depending on the results of the assessment, patients will be encouraged to spend the day in a chair rather than a bed and to take short walks on the floor.
With the Mobility Redesign, White says, “We want to change expectations a little bit. We need to encourage people to be mobile and not give them unconscious or conscious cues that they should lie in bed. We don’t want older adults to come to the hospital and get deconditioned.”
Duke Regional is also leading the way in workforce development. A large portion of nurses and CNAs at Duke Regional have trained to become Geriatric Resource Nurses (GRNs) or Geriatric Patient Care Advocates (GPCAs). The GRN and GPCA programs are offered by the Duke Center of Geriatric Nursing Excellence (CGNE) in collaboration with DUHS Clinical Education and Professional Development.
“We provide education so staff have increased competency and confidence in caring for older adults who often have complex and unique needs,” says Loretta Matters, MSN, RN-BC, associate director of the Duke CGNE.
Participants learn about geriatric syndromes, medication management, and mobility, as well as strategies to help communicate with and care for older adults, such as moving slowly, speaking in a lower pitch, and using a hand-under-hand technique to encourage and “remind” dementia patients to feed themselves.
Meanwhile, geriatricians Serena Wong, DO, medical instructor, and Milta Little, DO, associate professor of medicine, are promoting interdisciplinary teams for older patients at Duke Regional.
“I’m really excited,” Wong says. “Milta and I are working on implementing a new kind of group rounds based on an interprofessional team involving nursing, physical therapy, occupational therapy, speech therapy, pharmacy, and geriatrics.”
Little explains: “The care needs tend to be so complex, it takes more than just one person and one lens to be able to manage all of those effectively. The interprofessional team is a critical piece of geriatric medicine and will be a critical piece of any initiative at Duke Regional moving forward.”
This story was written by Mary-Russell Roberson, a freelance writer in Durham. She covers the geriatrics and aging beat for the Department of Medicine in the Duke University School of Medicine.
[Photo: Allison Kiefer, center, a clinical team lead in the Duke Regional Hospital Emergency Department, is trained as a Geriatric Resource Nurse]