From the Director

Countdown to the basketball game! Get ready for some trash-talkin’, Ani-bashing (well, that is from McManigle), sweat-flying, attending Achilles tearing, you-get-a-chance-to-play-in-Cameron hoops! Serious thanks to Ani Kumar, Div Patel and Tony Galanos, as well as Madi, for planning the ?th Annual Faculty-Housestaff Basketball game. See you there Thursday night!
In other goings-on …. SARS, check that procedure log! Update it and please let the chiefs and me know if you are in need of any procedures. The ABIM doesn’t joke around much, and we need these to be complete for you to sit for boards.
We will be having our first annual Intern and JAR class retreats coming up (May 31 and June 1). These half day retreats, held off campus, will be a way to deliver some class specific programming (being a team leader, interview skills, etc) as well as getting some structured work done on issues important to you. The chiefs have been working hard to secure coverage (and thanks to all who are helping). More details to follow in the next week!
Thank you to our “Make Noon Conference Great Again” committee for working on guidelines, schedules, etc to improve our education. I was away at the PD’s meeting but I hear that Lish Clark did an awesome noon conference on HHS/DKA using cases, audience participation, etc. This is our GOAL for noon conference – definitely worth watching this one.
Lots of kudos this week! Kudos to Pascale Khairallah, David Sermer and Jordan Pomeroy from Matt Kappus for great work in the MICU, with extra kudos to David from Pascale for being an awesome call-buddy. Kudos to Matt Atkins from Lindsay Boole for helping medical students Patrick O'Shea and Elliot Le win the medical school QI symposium for the paging project, and to the other medical students representing at the QI symposia – Stephanie Pagliuca and Noelle Kelly. Also to Zach Wegermann for really stepping up when a colleague was in need, and to the entire VA team from Chris Hostler for being fantastic about patient care during the busiest VA weeks of the year – Eric Black-Maier, Azalea Kim, Steph Li, John Musgrove, Ryan Orgel, John Paul Shoup, Jenny Van Kirk, Anne Weaver, Manisha Bhattacharya, Amanda Boyd, Stephen Kimani, Phil Liu, Jared Lowe, Dan Maselli and Maggie Moses, as well as dayfloats Ben Peterson and Bhavana Singh. Thanks everyone!
This week’s pubmed from the program goes to Adam Barnett for his article in Circulation: Arrhythmia and Electrophysiology with mentor Jon Piccini .. “Recent Advances in Lesion Formation for Catheter Ablation of Atrial Fibrillation” Barnett AS, Bahnson TD and Piccini JP.
Have a great week!
Aimee
What Did I Read This Week?
Submitted by David Butterly, MD
Survival Benefit with Kidney Transplants from HLA-Incompatible Live Donors Orandi, Luo, Montgomery, Segev et.al. NEJM 2016; 374: 940-950
This article appeared in the March 10th addition of the NEJM. We recently reviewed this in Nephrology Journal Club which gave me the chance to read it in more detail. Duke was a participating center and Dr. Deb Sudan (Transplant Surgery) was the PI here. The authors – several at Hopkins – have a long track record of similar research in this area and have previously published their single center experience with HLA and ABO incompatible transplant recipients.
Background:
Approximately 25 million Americans have CKD and nearly one million have ESRD. Of those affected with ESRD, 700,000 are managed with dialysis and nearly 300,000 with kidney transplantation. Transplantation not only leads to a benefit in quality of life for our recipients but also a significant reduction in mortality. As demonstrated by Wolfe et.al. in their seminal work published in 1999 in the NEJM, the expected increase in life expectancy conferred by kidney transplant is roughly 10 years overall and ranged between 3 and 17 years according to patient group. There are nearly 100,000 patients on the UNOS list awaiting transplantation in the US and a substantial subset of them (more than 30,000) have detectable ant-HLA antibodies. Patients become “sensitized” to HLA antigens by prior exposure thru blood transfusion, prior organ transplantation, and pregnancy. These sensitized patients incur substantially longer wait times on the UNOS list along with a higher risk of mortality awaiting transplantation.
The best option for all of our patients remains a compatible living donor, but for those highly sensitized patients this becomes increasingly hard to find. New advances to “desensitize” or remove allo-antibody and thus allow transplantation to proceed have been published over the last several years. Desensitization involves the use of treatment regimens that decrease preformed antibody levels directed toward the potential donor. Many different approaches have been used, however, most combine plasmapheresis, IVIG, rituximab, and bortezomib along with early initiation of maintenance immune suppression.
Present Study:
This study reports the results on a large cohort of these patients who were able to successfully proceed with transplant from an HLA incompatible donor after desensitization and compared their survival to two matched groups awaiting transplant. 1025 patients were enrolled at 22 centers in the US between 1997 and 2011. Antibody detection methods are described in Table 1 and each participating center classified the recipient antibody level as low, medium, or high. Patients with anti-HLA antibodies who were also ABO incompatible made up 5.8% of the cohort.
Each of the 1025 recipients were matched to 5 patients from the SRTR data base who were wait-listed and subsequently received a deceased donor kidney (wait-list-or-transplant) and another 5 patients who were wait-listed and never received an organ (wait list only). Survival in each of the groups was tracked. Of the 1025 patients, 185 had lower donor antibody, 536 moderate, and 304 high. The characteristics of each of these patient groups are shown in Table 2. As one would expect, those in the most sensitized group (Positive Cytotoxic Cross-Match) had the highest Panel reactive antibody and had the longest duration of dialysis prior to transplant.
The characteristics of the study group compared to the 5125 in each of the 2 control groups are shown in Table 3. Mean PRA (panel reactive antibody) was similar at 66-68% and roughly 40% in each group had received a previous transplant.
The crux of the study is demonstrated in the next figure and tables. Overall survival of each groups are shown in Figure 1 along with Table 4. Recipients of Incompatible kidneys had superior survival at 1, 5, and 8 years compared to each of the control groups:
1 year: 95 v 94 v 89.6%
5 year: 86 v 74 v 59.2%
8 year: 76 v 62 v 44%.
There was an absolute increase in the survival of 13.6% and 32.6% seen in recipients compared to the two control groups. This survival benefit was demonstrated across Cross Match Strengths as shown in Figure 2.
Conclusion:
The strengths of the study include large sample size and duration of follow up along with the multicenter design. One of the problems with the study is that it is not a randomized controlled trial- but I would argue that a RCT addressing this question is unlikely to ever be done- and this might be the best data we get. Another problem is that the desensitization protocols were not uniform across centers or eras as approach to these patients has changed as newer agents have come to market.
These sensitized recipients remain at increased risk for rejection even after desensitization protocols are employed. Additionally, desensitization protocols increase the overall level of immunosuppression in the recipient and therefore increase the later risk of infection and malignancy. Finally, these drugs (Bortezimab, Rituximab) and procedures (PLEX) are expensive and use in these protocols represent off-label use for the agents and thus would need buy-in from payers or the generalizability will remain limited.
With these caveats, these authors were able to demonstrate a clinically significant survival benefit in this cohort of sensitized patients and I think these data can help us as we guide our allo-sensitized patients in their treatment options when moving forward with tra
QI CORNER
Want to be the next Clark, Schulteis, or dare I say.... Bae?
Apply to the GME Concentration in QI!
Info: http://sites.duke.edu/gmeconcentrations/
Application: https://duke.qualtrics.com/jfe/form/SV_3aTKSoFgwd8JteB

And if you REALLY love QI, think about applying for this Chief Resident for Quality and Safety job. Open to current JARs and SARs (SARs--with approval from your fellowship program director, if applicable). Formal application will be out soon, but please go ahead and talk to me or Joel Boggan now if this is on your radar.
CLINIC CORNER

Hey everyone!
Gen Med Careers Night has been rescheduled to May 3!!
Mark your calendars for May 3rd, 6:30-8:30 pm, Med Res Library! Sharon Rubin is organizing a career planning social event, dinner will be served. Whether you are considering hospital medicine, primary care, or academic general internal medicine (including health services research, quality improvement, education or administration) please join us for food and drink and networking. All years are welcome, come and hear from a diverse faculty panel.
ACLT Updates
The current ACLT group is preparing for their DC advocacy trip May 17-18! They have honed their message for legislators around the important issue of opioid prescribing, and will be advocating for improvements in integrating information technology to improve safe prescribing as well as better access to non-opioid modalities for pain management. Look for their one page take-away handout soon.
Schedules, schedules, schedules
If you have any questions about yours, please let Armando, Jen, Lynsey and myself know – we are here to help!
See y’all in clinic!
From the Chief Residents
Grand Rounds
Friday, April 29 - Special Speaker - Coach Cutcliffe
Noon Conference
| Date | Topic | Lecturer | Time | Vendor |
| 4/25/16 |
MKSAP GIM |
|
2002/12:00 | Domino's |
| 4/26/16 |
Ambulatory Town Hall |
2002/12:00 | Mediterra | |
| 4/27/16 |
Obesity and Weight Management |
William Yancey |
12:00 | Cosmic |
| 4/28/16 |
Maestro Care |
Jon O'Donnell & David Claxton |
12:00 |
Chick Fil A |
| 4/29/16 |
Research |
12:00/2002 | Panera |
From the Residency Office
Stead Sponsored Event
This is an opportunity for drinks, appetizers and to hear from some of our great faculty about how they manage to wear all the "hats" of an academic clinician. Everyone is invited, please just let Lish Clark know if you will attend so we can make sure to provide enough food/beer/wine. Hope to see you there!!
Thanks
Alicia Clark, MD
MEDICAID EXPANSION AND REFORM: A LEGISLATIVE FORUM: Tuesday, April 26, 2016
On Tuesday April 26 from 6:30 - 8:30 at NCCU there will be a gathering of local legislators and leaders from the Durham health sector (DUHS, Health Department, Senior PharmAssist) discussing Medicaid expansion and reform. It's a great opportunity to learn more about proposed changes that could impact many of our patients.
Please see PDF file attached at the end of this post for more information.
Abstracts Are Due May 1st!
Our annual Resident Research Grand Rounds is a wonderful opportunity for you to display and share results of your research projects.
We invite and encourage you to:
1)- Submit an abstract for the Califf Resident Research award competition and
2)- Display a poster of your research on May 20th during Resident Research Grand Rounds. You can use the same poster from a previous meeting.
The abstract is due on May 1, 2016 (please see instructions below)
Resident Research Grand Rounds is on May 20, 2016 at the SEARLE Center beginning at 7 am, with talks 8-9 am
Please contact murat.arcasoy@dm.duke.edu with any questions.
Califf Medicine Resident Research Award Prizes (3 oral presentations)
1st place $1000
2nd place $500
3rd place $250
2 Best poster awards $250- One clinical research poster and one QI project poster
Instructions for abstract submission on May 1st for the Califf Resident Research Award Competition
Abstract format
Authors: The resident is the first author and presenter (poster or oral presentation)
Faculty sponsor (research mentor):
Title:
Background:
Methods:
Results:
Conclusions:
Support (funding source if applicable): eg Faculty Resident Research Grant or Stead Grant
Limit – 300 words maximum (including title, background, methods, results and conclusions).
One Table or one Figure is allowed in addition to the 300 words.
Supporting letter from Research Mentor is addressed to:
“The Califf Medicine Resident Research Award Committee” and
emailed to Dr. Arcasoy along with the abstract please murat.arcasoy@dm.duke.edu
Schwartz Center Rounds
Title: “Life After Death: A Donor Mom Shares her Son’s Legacy”
Panelists:
Ms Delores Benton Evans - Donor mom and kidney recipient
Nancy Knudsen, MD - Co-Director, SICU
Debra Bird - Organ Donation Coordinator with Carolina Donor Services
Lindsay Stietzel - Family Support Coordinator with Carolina Donor Services
Wednesday, April 20, 2016, Noon - 1 p.m., Duke North 2002 Lecture Hall
About Schwartz Center Rounds:
All members of the Duke Medicine community are invited to attend an ongoing series of discussions called the Schwartz Center Rounds about the human side of patient care. Schwartz Center Rounds is a monthly interdisciplinary conference that offers all of us from no matter which discipline as well as non-clinicians who work closely with our patients a regularly scheduled time.... We are excited to have brought this program here to Duke and hope many of you will be able to join us on a regular basis.
Please contact, Lynn Bowlby, MD (lynn.bowlby@duke.edu), or Nathan Gray, MD (nathan.gray@dm.duke.edu) with questions. There is no need to RSVP, but we do recommend that you arrive early as food and seats are at a premium!
Office Hours for Dr. Zaas
Dr. Zaas will have the following office hours. Please feel free to stop by during these times and of course always feel free to reach out to her office to set up a meeting outside of these times if needed!
Monday - 3:00 p.m. to 4:00 p.m.
Thursday 10:00 a.m. to 11:00 a.m.
General Internal Medicine Career Night
General Internal Medicine Career Night
Interested in a career in General Internal Medicine?
Thinking about primary care medicine, Gen Med fellowship or hospitalist medicine?
Envision working in academics, research, Quality Improvement
or a combination?
Come to Gen Med Career Night
Tuesday May 3, 2016
6:30-8:30pm
Gen Med Resident Library
Dinner from Nosh
Come ask questions for our panelists about their path and journey:
Kevin Shah, Claire Kappa, Sharon Rubin, David Edelman, Sonal Patel, Lance Teagen, David Gallagher and Daniella Zipkin
Please RSVP to Sharon.rubin@dm.duke.edu by May 2, 2016
Please see flyer at the end of this post
Charity Auction 2016
The Internal Medicine Residency program Charity Auction, benefiting Senior PharmAssist will take place Friday, April 29th, 2016 @ 7:00 p.m. at Motorco in Durham! Tickets will go on sale in early April. We look forward to seeing you there. Please see the flyer at the end of this post!
LiveSafe Mobile App
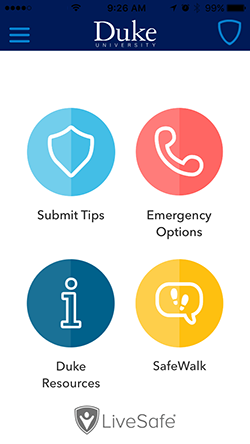
Duke is introducing a new mobile app called LiveSafe to put a powerful safety tool in the hands of the Duke community.
The app, available as a free download from Apple and Android app stores, enables smartphone users to submit real-time tips to Duke Police, virtually “SafeWalk” friends and family while traveling, place emergency calls, and access important resources for support.
You can find more information, including instructions on how to download the free app, on the DukeALERT website: http://emergency.duke.edu/notified/livesafe.
Opportunities for Wellness
Feeling down? Need to talk to someone?
All trainees at Duke have FREE access to Personal Assistance Services (PAS), which is the faculty/employee assistance program of Duke University. The staff of licensed professionals offer confidential assessment, short-term counseling, and referrals to help resolve a range of personal, work, and family problems. PAS services are available free of charge to Duke faculty and staff, and their immediate family members. An appointment to meet with a PAS counselor may be arranged by calling the PAS office at 919-416-1PAS (919-416-1727), Monday through Friday between 8:00 A.M. and 5:00 P.M. For assistance after hours, residents and fellows can call the Blood and Body Fluid Hotline (115 inside DUH, 919-684-1115 outside) for referral to behavioral health resources. Another resource is Duke Outpatient Psychiatry Referrals at (919) 684-0100 or 1-888-ASK-DUKE.
https://www.hr.duke.edu/pas/
Upcoming Dates and Events
April 28 - Annual Faculty vs Resident Basketball Game
April 29 -Charity Auction
May 14 - Spring Picnic
May 20 - Resident Research Grand Rounds
May 20-21 - 2nd Annual Family Weekend
May 31 - Rising JAR Retreat
June 1 - Rising SAR Retreat
June 4 - SAR Dinner
Useful links
GME Mistreatment Reporting Site
https://intranet.dm.duke.edu/influenza/SitePages/Home.aspx
http://duke.exitcareoncall.com/
Main Internal Medicine Residency website
Main Curriculum website
Department of Medicine
Confidential Comment Line Note: ALL submissions are strictly confidential unless you chose to complete the optional section requesting a response
Opportunities
www.bidmc.org/CentersandDepartments/Departments/BIDHC
http://www.careermd.com/employers/latestbulletins.aspx