From the Director

Happy August! Block 1 is officially in the books for JARs and SARs! Fellowship interviews are rolling in for the SARs and we just finished a very well done Physical Exam Week! Thank you to Murat Arcasoy, as well as our “Physical Exam Models” Zach Wegermann, Div Patel, Winn Seay and Bill McManigle.
This week, we have our first RESILIENCY CONFERENCE, led by Med Psych residents Jake Feigal and Jim Lefler. This conference is for housestaff only and is the first in what will be an ongoing curriculum throughout the year. I have no doubt that it will be excellent, so please make every effort to attend.
Lots of kudos this week … to Alana Lewis and Kristen Glisinski for being great dayfloats at the VA (from Azalea Kim), to AJ Blood, Andy Chen, Emily Mao, Mohammed Raad and Pierre Elias for great work on cards consults (From Jordan Pomeroy), to Dan Maselli for calling GI consultant and Class of 2015 alum Iris Vance with very well described consults (from Iris!), to CoCo Fraiche from Jon Bae for doing a great job on 1010, and to the entire night resident team (Coco Fraiche, Kahli Zietlow. Linda Koshy and Pascale Khairallah) from fellow night resident Maggie Infeld for being a great team, and to Sarah Goldstein from the night float crew for her great advice and assistance. Also a belated kudos to Eric Yoder from the DOC team for helping out a colleague who was swamped!
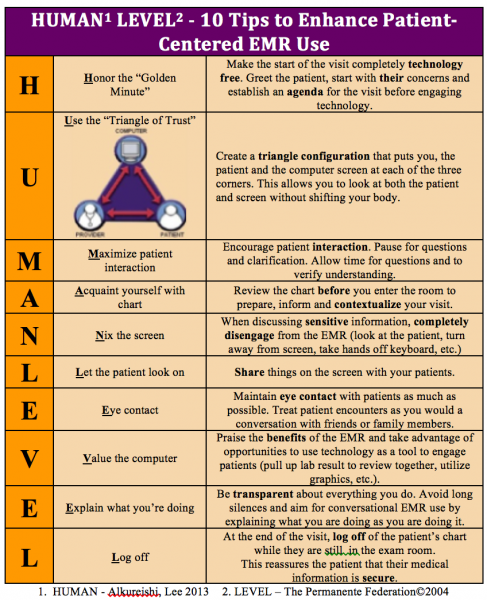
If you made to Grand Rounds on Friday (or if you missed it), there was some provocative conversation regarding patient communication. We are all always working to be better at connecting with our patients and providing the care that they need. Tom LeBlanc (Duke grad, past VA Chief and current Heme-Onc/Pall Care attending) sent an article (attached at end of updates) and Jon O’Donnell sent the mnemonic (see below) as some helpful hints on how to incorporate the electronic health record and the computer into our daily interactions with patients. Overall, I couldn’t be more proud of how well you all connect with your patients (some examples are Mike Dorry’s invitation to his clinic patient’s funeral during intern year – he made a connection in a very short time, Jesse Tucker driving a patient home who didn’t have a ride, and Andrea Sitlinger receiving this beautiful quilt from her patient at the DOC). I know there are more examples as well of the impact you make on a daily basis.

This week, we have the INTERN-CHIEF Happy Hour at Alivia’s on Thursday night! Come on out and join us, and keep your calendars marked for the Summer Celebration on Aug 21st!
This week’s pubmed from the program goes to Jessie Seidelman for her abstract that was accepted to ID Week! "Consensus Definition of Clostridium Difficile Infections That Are Not Preventable by Antibiotic Stewardship Programs”. Mentor is Dr. Luke Chen.
Have a great week!
Aimee
What did I read this week?
Submitted by Dr. David Butterly
Mild Chronic Hyponatremia in the Ambulatory Setting: Significance and Management
Helbert Rondon-Berrios and Thomas Berl Clinical Journal of the American Society of Nephrology
This article appeared in a recent issue of CJASN and is a nice review of a common and clinically important topic. The authors are experts in the area of hyponatremia and have published extensively in this area. The article provides a nice review of recent data analyzing the clinical significance, presentations, impact on morbidity and mortality, and treatment of hyponatremia.
In hospitalized patients, hyponatremia is associated with higher mortality across a number of etiologies including CHF, Cirrhosis, Cancer, CKD, and in patients admitted to the ICU for any reason. Several studies highlighted here have examined this association in outpatients. These four studies (Table 1) found an adjusted mortality risk of 1.21 to 3.56 HR in hyponatremic patients. In the largest cohort, Mohan looked at PNa in 14,697 patients participating in the NHANES study. Hyponatremia was seen in roughly 2% of participants and was associated with a HR of death of 3.61. Taken together, these data strongly suggest that hyponatremia is associated with increased risk of mortality in outpatients, as it is in hospitalized patients.
Is asymptomatic hyponatremia truly asymptomatic? The adaptive cerebral response to hyponatremia involves the loss of osmolytes, several of which are neurotransmitters, making the association of hyponatremia and central nervous system alterations (neurocognitive deficits, gait disturbance, etc) biologically plausible. These associations are highlighted in the next sections and tables of this paper.
Neurocognitive
Table 2 details the 3 trials highlighted which evaluated the association of chronic hyponatremia and neurocognitive deficits. All 3 studies highlighted found changes in patients with hyponatremia. In a very interesting study included in the section, Renneboog performed neurocognitive testing on 16 patients with SIADH. In this study, each patient served as his/her own control and were compared before and after correction of hyponatremia. Attention deficits were evaluated by measuring reaction times and errors to a series of auditory and visual stimuli. When hyponatremic, the mean latency along with the error numbers increased and were statistically significant when compared to the patient scores when Na had been corrected. The study went on to compare the outcomes when tested in a group of volunteers with moderate alcohol intake, and in fact the hyponatremic patients scored worse than these volunteers.
Gait Disturbance
Another component of the study by Reeneboog evaluated gait disturbance in this same cohort. Patients were asked to do a tandem walk on a pressure sensitive calibrated platform. With this measurement, the closer the tracing is to a straight line, the more normal the reading. Figure 1 shows examples in 3 representative patients. Studies on the left were obtained with the serum Na ranging from 124-130. Those same three patients repeated the study when Na was corrected and ranged from 135-139. Again, the readings obtained in the hyponatremic patients were worse than those in normal volunteers with moderate alcohol intake.
Falls
It is probably not surprising to anyone that given the neurocognitive deficits along with the gait disturbance that hyponatremic patients are at increased risk for falls. This indeed seems to be the case. Three studies highlighted in Table 3 have examined this and fall risk increased from 1.32-9.45 fold in these studies. To study the clinical significance of the demonstrated gait disturbance, Renneboog and colleagues studied the prevalence of falls in 122 hyponatremic patients and compared them to 244 age matched controls over a 3 year period. Hyponatremia was associated with a higher prevalence of falls with an OR of 9.45. The threshold at which fall risk increased was a serum Na of 134.
Fractures and Osteoporosis
Table 4 outlines the 6 studies which have examined the association of fracture risk and hyponatremia. Again, serum Na decreases that seem pretty mild (131-133) were associated with increased relative risk of 1.34 to 4.8. This increased fracture risk seems to not only be due to the gait instability and fall risk but also associated osteoporosis. In another study using the NHANES database, hyponatremia (mean Na 133) was associated with increased relative risk of osteoporosis of 2.87.
Treatment
In the final 4 pages, options for treatment including fluid restriction, increasing solute load, loop diuretics, demeclocycline, and Vasopressin Receptor Antagonists are covered. This section includes an excellent review of the physiology of Loop Diuretics actions and why they are not commonly associated with hyponatremia. Finally, the data from the SALT1 and SALT 2 trials (NEJM 2006) are reviewed.
In conclusion, mild hyponatremia is not as benign as once thought and is associated with increased morbidity and mortality. Neurocognitive deficits, gait instability, and falls along with fractures are a common presentation. I hope you enjoy this review of the topic as much as I did.
QI CORNER
Dr. Lindsay Boole, VA QI Chief Resident
Please join us NEXT Wednesday, August 12 at 5:30pm in the Med Res Library, for the second PSQC meeting of the year!
The Patient Safety and Quality Council is our internal (within the residency program) group focused on patient safety and quality improvement. Every year, we choose several QI projects at the beginning of the year and work together to execute them. An impressive number of abstracts, posters, and manuscripts have come out of the work of this committee. Plus, this is YOUR opportunity to get involved and improve the care we deliver at Duke!
Our first meeting, at Six Plates, was a big success. We brainstormed dozens of project ideas, with focuses ranging from traditional clinical QI, to improving communication between residents and nurses, to targeting patient satisfaction, to improving resident quality of life. At the August meeting, we’ll start to narrow our focus and get closer to selecting a few feasible projects for the year.
To sweeten the deal, we’ll lure you with free dinner at the meeting.
Looking forward to seeing many of you there NEXT Wednesday!
From the Chief Residents
Grand Rounds
Friday, August 7- Infectious Disease, Micah McClain
Noon Conference
| Date | Topic | Lecturer | Time | Vendor |
| 8/3/15 | SAR Emergency Series: Bradyarrhythmias |
Jonathan Buggey |
12:00/2002 | Domino's |
| 8/4/15 | SAR Emergency Series: Diabetic Emergencies: Hyperglycemia/Hypoglycemia |
Adva Eisenberg |
12:00/2002 | Mediterra |
| 8/5/15 | SAR Emergency Series: Electrolyte Disorders - Hyperkalemia and Hypokalemia |
Joanne Wyrembak |
12:00/2002 | China King |
| 8/6/15 | QI Patient Safety Noon Conference- Intro to Resilience |
Jim Lefler and Jake Feigal |
12:00/2001 |
Subway (Residents Only) |
| 8/7/15 | Chair's Conference | Chiefs | 12:00/2002 | Firehouse Subs |
From the Residency Office
STEAD TREAD 2015!
Wanted to take a second to invite you all to come support the Stead Tread, the Kempner Stead Society's annual charity event, which benefits Lincoln. It was a blast this year, and since we're due for some good weather this year, I'm sure it will be even better this time around.
Some additional information:
Please access the Stead Tread 2015 website (http://www.steadtread.org) for additional information, to securely register ($25), or make a donation
Race date/time: Saturday, September 12th, 2015 at 10:00AM (registration from 8:45-9:45)
Race location: American Tobacco Trail, starting at Solite Park on Fayetteville Road in Durham (https://www.google.com/maps/place/Solite+Park/)
Race beneficiary: Lincoln Community Health Center (and all Lincoln patients walk/run for free)
Your $25 registration fee includes an official Stead Tread 2015 T-shirt – shirts are going fast, so register ASAP to reserve your size!
Participants are welcome to run or walk, and strollers are permitted - kids under 12 walk/run for free (but should be registered by their parent/guardian)
In case you cannot make the race this year, donations can be made securely through our website
Thank you for considering supporting the Stead Tread – we really hope to see you there this year. For any questions, please contact us through our website (http://www.steadtread.org), via e-mail at steadtread5K@gmail.com, or by replying directly to me (Matt Crowley, M.D. <matthew.crowley@dm.duke.edu>).
SARs
Please know there is an excellent opportunity to hone your interviewing skills. Dr. Kathryn Pollak who is a communication coach and faculty member in the SoM will provide 4 1-hour sessions from which you can choose. In the session, Dr. Pollak will cover tips to finesse interviewing skills as well and give some a chance to role play. She also will be available for practice for their interviews in September and October.
The four sessions will be held the following dates and times:
Monday, August 17th: 12:00 noon to 1:00pm
Tuesday, August 18th: 4:00 to 5:00pm
Wednesday, August 26th: 12:00 to 12:00pm
Thursday, August 27th: 4:00 to 5:00pm
Each session will be 10 people or less, that way it’s more personalized. Please let me know as soon as possible which session you would like to sign up for. This is a very valuable tool being offered!
Upcoming Dates and Events
August 21 - Housestaff Welcome Event
September 12 - Stead Tread
Useful links
https://intranet.dm.duke.edu/influenza/SitePages/Home.aspx
http://duke.exitcareoncall.com/
Main Internal Medicine Residency website
Main Curriculum website
Department of Medicine
Confidential Comment Line Note: ALL submissions are strictly confidential unless you chose to complete the optional section requesting a response
Opportunities
http://www.ad001.info/blasts/CKS/CKS15_05431/CKS15_05431.html