From the Director

Well, not the best night if you are a Panthers fan, but Duke-State was a bright spot (and in my opinion, so was UNC-Notre Dame :>). We are entering our second week of Fun-bruary this week, so be on the lookout for more trivia as well as random acts of kindness. Congrats to Gen Med 3 (Amanda Verma, Meg Steiner, Kelly Ground) for winning the Friday Starbucks run (they sent me a top 10 list of why they were deserving) and to Aly Shogan for winning Dr. Klotman’s Duke tickets. More fun to be had this week for sure.
Big giant amazing kudos to Amy Jones, Anubha Agarwal, Lakshmi Krishnan and Dinushika Mohottige for initiating and planning and pulling off the first (of many) Duke Narrative Medicine Project writers weekends! For those of you who were able to hear our guest speaker Dr. Anna Reisman at Grand Rounds, you got a taste of the power of writing in medicine. Many thanks to our faculty participants Ray Barfield, Tony Galanos, David Pisetsky and Frank Neelon, as well as to Dr. Reisman for their time and mentorship. Pictures below. We are looking forward to the scholarly product from the weekend, and to also future narrative medicine work from this outstanding group. For those of you who didn’t know, Amy Jones wrote the GME Innovations Grant for the Narrative Medicine Workshop as part of her participation in the Resident as Teacher GME Concentration. Outstanding!



Other kudos this week to Winn Seay for Chair’s Conference and to everyone who provided outstanding participation. Love having conference back in the Med Res library!
If you haven’t had a chance to read it yet, Murat has summarized the results of the FIRST trial (the surgery iCOMPARE) in this week’s WIRTW. AAIM (which is our academic internal medicine professional society) is busy writing a position paper to the ACGME regarding this same topic. While we won’t know results from iCOMPARE for awhile, the position paper is attached. These are both worth a read as we are part of the GME community.
Other reminders to SARs to register for the ABIM exam (aka boards) before the price goes up. If you are starting to participate in the Global Morning Report emails, this is a quick and easy way to get a little studying in. Advisors will be reaching out to ask you about your study plans, so be aware and be thinking about this. Your ITE scores and reports are in your Medhub file, so it is easy to take a look and see where you should focus your time. As a word of caution - don’t anticipate lots of study time during your first two months of fellowship/job!
Our second (repeat of Feb 2) readiness for fellowship meeting will be held TOMORROW (Feb 9) at 6pm in the Med Res library. Great attendance last week, so please come if you were unable to join us on the 2nd.
Kudos this week go to our program’s alum Dr Bibhu Mohanty for his narrative piece just published in the Journal of Graduate Medical Education- Thoughts at the Groin Bibhu Mohanty JGME February 2016. Bibhu D. Mohanty. This same issue of JGME also had a paper by IM prelim/Duke Rads alum Lars Grimm and Med Peds alum/faculty Carolyn Avery!
Have a great week
Aimee
What Did I Read This Week?
Submitted by Murat Arcasoy, MD
National cluster-randomized trial of duty-hour flexibility in surgical training. NEJM February 2, 2016, by Bilimoria and colleagues. Flexibility in Duty Hour Requirements
for Surgical Trainees (FIRST) Trial.
Why did I read this article
The FIRST trial is of great interest to all of us because our Program is participating in the iCOMPARE trial (Comparative Effectiveness of Models Optimizing Patient Safety and Resident Education) for Internal Medicine residency programs.
What did the authors do
In a non-inferiority design, General Surgery residency programs (n=117) were randomized to current ACGME duty-hour policies or more flexible policies that waived rules on maximum shift lengths and time off between shifts. Primary outcome was 30-day postoperative death or serious complications. Other outcomes included other postoperative complications, and resident perceptions and satisfaction regarding their well-being, education, and patient care.
What did the authors find
Data from 138,691 patients were analyzed. Flexible, less-restrictive duty-hour policies
were not associated with an increased rate of death or serious complications (9.1% in the flexible-policy group and 9.0% in the standard-policy group, P = 0.92; unadjusted odds ratio for the flexible-policy group, 0.96; 92% confidence interval, 0.87 to 1.06; P = 0.44; non-inferiority criteria satisfied) or of any secondary postoperative outcomes studied. Among 4330 residents, those in programs assigned to flexible policies did not report significantly greater dissatisfaction with overall education quality (11.0% in the flexible policy group and 10.7% in the standard-policy group, P = 0.86) or well-being (14.9% and 12.0%, respectively; P = 0.10). Residents under flexible policies were less likely than those under standard policies to perceive negative effects of duty-hour policies on multiple aspects of patient safety, continuity of care, professionalism, and resident education but were more likely to perceive negative effects on personal activities. There were no significant differences between study groups in resident-reported perception of the effect of fatigue on personal or patient safety. Residents in the flexible-policy group were less likely than those in the standard-policy group to report leaving during an operation (7.0% vs. 13.2%, P<0.001) or handing off active patient issues (32.0% vs. 46.3%, P<0.001).
Conclusion
As compared with standard duty-hour policies, flexible, less-restrictive duty-hour policies
for surgical residents were associated with non-inferior patient outcomes and no significant difference in residents’ satisfaction with overall well-being and education quality.
Remarks
I tried to imagine the challenge for a surgical resident who may need to “leave during an operation” to comply with restrictive duty-hour rules. That fewer surgical residents had to do so when randomized to the flexible duty-hour arm without compromising patient outcomes is a positive finding. Of course, there could be differences in outcomes not measured in this trial. I cannot wait to see the results of the iCOMPARE trial. As you know, our Program has been randomized to the flexible duty-hour arm. The iCOMPARE participating programs are listed in this link: http://www.jhcct.org/icompare/showassignments.asp
QI CORNER
This feature will return next week!
CLINIC CORNER

Hi all—
The changes, and this video , are good.
We have made some changes to a couple of In Basket folders to help improve workflow and make It easier for providers and clinical staff to know how best to use the EPIC functions. If you would like additional help, here are some additional options!
· Try watching this 7 minute video made by David Claxton from the Concierge team: In Basket Changes Video Quick Tip
· Schedule time with a concierge trainer. Their contact information is at the bottom of this email.
· Attend a Thrive Class. Class times and schedule is at the bottom of this email.
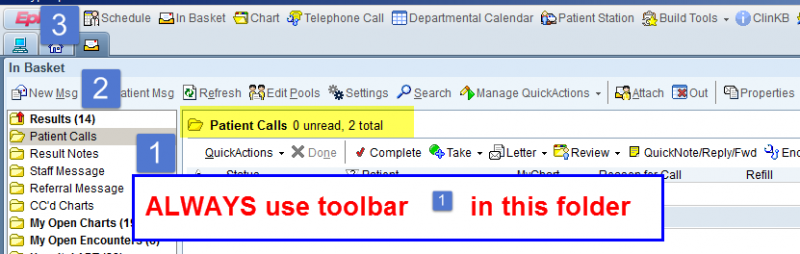
First, there is a cardinal rule for ALL In Basket folders: Always use the Toolbar within the folder to manage items in that folder (the lowest one, designated by in the screenshot below). Using this toolbar will save you clicks.
Here are the changes we have made for 2/4/2016:
1. Patient Calls folder-
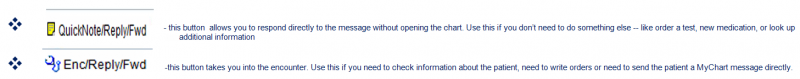
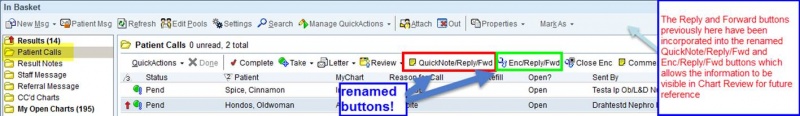
We have changed the names of two of the buttons to help you how to quickly respond to messages you receive.
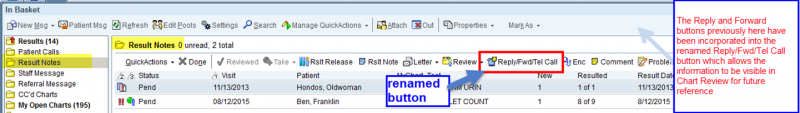
2. Result Notes folder-
We have changed the name of the Tel Call button to show you how to quickly respond to messages you receive.
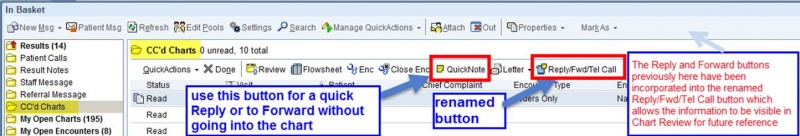
3. CC’d Charts folder-
We have changed the name of the Tel Call button here as well to help you quickly respond. Use the Quick Note button if you can reply without needing additional information. Use the Reply/Fwd/Tel Call button if you need to do anything else within the chart, like review information, write orders, look at problem list.
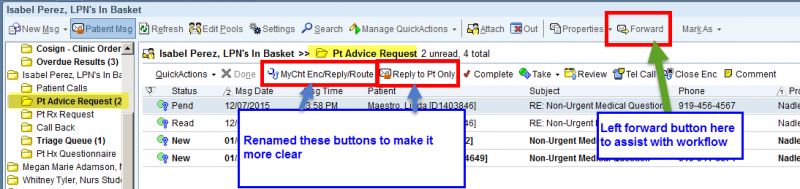
4. Pt Advice Request folder-
We have changed the name of the MyCht Enc button to show you how best to respond to messages you receive. Use the “Reply to Pt Only” button if you can respond back to the patient directly without additional information. Use the “MyCht Enc/Reply/Route” button if you need to do anything else within the patient’s record, like review information, write orders, or route to your clinical staff.
_____________________________________________________________________________________
This section is for Primary Care ONLY. If you are not a PCP, you will not see these folders.
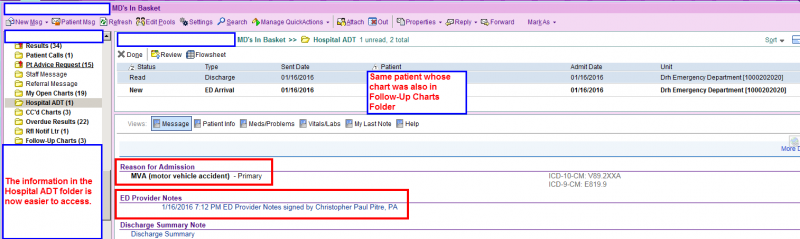
5. Follow-Up Charts folder-We are going to remove the folder called Follow-up Charts starting on 2/4/2016, because this information is also seen in the Hospital ADT folder, where you receive notification for the ED Arrival and Discharge. This Follow-Up Charts folder currently only goes to the PCP and is only for patients who have been seen and discharged from the Emergency Department.

Just as a reminder, we have also made recent changes to the Hospital ADT folder to allow providers to access the visit information more quickly.
_______________________________________________________________________________________________________________________________
If you would like more help using Maestro most efficiently, here are two options:
1. Contact one of the Provider concierge group for one on one assistance:
· Angela Anderson <angela.anderson@dm.duke.edu>;
· Carmen Taylor <carmen.taylor@dm.duke.edu>;
· David Claxton <david.claxton@dm.duke.edu>;
· Demarcus Simmons <demarcus.simmons@dm.duke.edu>
· Ally Hunter aeh50@duke.edu
2. Come take one of the Thrive Classes being taught at Duke Medicine Pavilion
2/16/2016 12:30-2 Tuesday DMP.2W91 - In Basket and Multi-provider schedule customization
2/26/2016 12:30-2 Friday DMP.2W91- Chart personalization and Documentation
3/15/2016 12:30-2 Tuesday DMP.2W91- Chart personalization and Documentation
3/30/2016 12:30-2 Wednesday DMP.2W93- In Basket and Multi-provider schedule customization
Lisa Nadler, MD
Primary Care Physician Champion
3. Care Managers—
Joan Levitt RN , for any Duke Well pt. On top banner it will say Duke Well—Medicare or Duke Basic/ Select.
She will go to pts homes.
Tomislava Racic RN for the same pts, but not as sick, without home visit needed.
Use them! They can help with transportation, meds, compliance….
Refer thru Meds and Orders like you would anything..and if you are not sure if they have Duke Well, they will figure it out!
Kenya is Medicaid Care manager, refer thru Marigny
4. Jodi Hewett, Temp Nurse Manager , goes back to Fam Med Feb 22.
There are applicants for the position, interviewing now.
5. New therapists starting on Feb 22 as part of project with Alliance Behavioral Health--
Joy Long and Ashley Cyr
you will see them with your pts during visits..
thanks all!!
Lynn Bowlby and Co.
From the Chief Residents
Grand Rounds
Friday, February 12 - Oncology, Dr. Steve Patierno
Noon Conference
| Date | Topic | Lecturer | Time | Vendor |
| 2/8/16 |
DNARs & MKSAP Renal |
Dr. David Turner |
12:00/DN 2001 | Nosh |
| 2/9/16 | Edema, Renal Syndromes, and Clinical Use of Diuretics |
Dr. John Roberts |
12:00 | Domino's |
| 2/10/16 |
ACGME Survey |
Dr. Zaas and Chiefs |
12:00 | China King |
| 2/11/16 |
Wellness / G-Briefing |
Jim Lefler and Jake Feigal/Dr. G |
12:00 |
Chick-Fil-A |
| 2/12/16 | Chair's Conference | 12:00 | Hungry Leaf |
From the Residency Office
Fellowship Program Info Sessions
Gastroenterology Fellowship Program
Monday, March 7th at 5:00pm in the Tyor Conference Room located in the GI Administrative Suite.
Hem-Onc Fellowship Program
March 1, 2016 4:00-5:00 PM. Room 405 Mudd (Conference Room). Pizza and drinks will be provided.
Teaching and Leading EBM: A Workshop for Educators and Champions of Evidence-Based-Medicine
Registration is now open!
Teaching and Leading EBM: A Workshop for Educators and Champions of Evidence-Based-Medicine
Duke Medicine, Durham NC
April 12-15, 2016
http://sites.duke.edu/ebmworkshop
This workshop focuses not only on learning EBM skills, but also on teaching EBM. Previous participants have included rising chief residents, faculty charged with developing an EBM curriculum, librarians, and other clinicians and faculty passionate about applying the best evidence to patient care. The program includes large group sessions in the morning, then supportive, small group, learner-driven sessions for the rest of the day.
The workshop will take place on the Duke Medicine campus in the new Trent Semans Center for Health Education and the Duke Medicine Pavilion.
Workshop Objectives:
Train leaders in medicine to facilitate evidence-based clinical practice in their teaching and practice settings.
Practice the skills involved in evidence-based medicine including clinical question formation and acquisition of medical evidence from the literature.
Review and develop critical appraisal skills and application of available evidence to patient care and medical education.
Develop skills in teaching EBM in both large and small group settings.
Provide interactive experience with a variety of evidence-based resources guided by faculty with expertise in evidence-based practice.
Please contact Megan von Isenburg (megan.vonisenburg@duke.edu) or Laura Huffman (laura.huffman@dm.duke.edu) with any questions.
11th Annual Duke Health Patient Safety and Quality Conference
REGISTRATION NOW OPEN: 11th Annual Duke Health Patient Safety and Quality Conference
11th Annual Duke Health Patient Safety and Quality Conference
Thursday, March 10, 2016
Durham Convention Center
301 West Morgan Street, Durham, NC
Onsite registration/check-in begins at 7:00 AM
Conference program is from 8:00 AM-4:30 PM
Register online today!
Schwartz Center Rounds
Panelists:
Jamie Veasey, PACE Nurse
Kelly Forrester, Case Manager
Margarita Bidegain, MD
Heather McLean, MD (Pediatric hospitalist)
Wednesday, February 17, 2016, Noon - 1 p.m., Duke South Amphitheater
About Schwartz Center Rounds:
All members of the Duke Medicine community are invited to attend an ongoing series of discussions called the Schwartz Center Rounds about the human side of patient care. Schwartz Center Rounds is a monthly interdisciplinary conference that offers all of us from no matter which discipline as well as non-clinicians who work closely with our patients a regularly scheduled time.... We are excited to have brought this program here to Duke and hope many of you will be able to join us on a regular basis.
Please contact, Lynn Bowlby, MD (lynn.bowlby@duke.edu), or Nathan Gray, MD (nathan.gray@dm.duke.edu) with questions. There is no need to RSVP, but we do recommend that you arrive early as food and seats are at a premium!
Opportunities for Wellness
Feeling down? Need to talk to someone?
All trainees at Duke have FREE access to Personal Assistance Services (PAS), which is the faculty/employee assistance program of Duke University. The staff of licensed professionals offer confidential assessment, short-term counseling, and referrals to help resolve a range of personal, work, and family problems. PAS services are available free of charge to Duke faculty and staff, and their immediate family members. An appointment to meet with a PAS counselor may be arranged by calling the PAS office at 919-416-1PAS (919-416-1727), Monday through Friday between 8:00 A.M. and 5:00 P.M. For assistance after hours, residents and fellows can call the Blood and Body Fluid Hotline (115 inside DUH, 919-684-1115 outside) for referral to behavioral health resources. Another resource is Duke Outpatient Psychiatry Referrals at (919) 684-0100 or 1-888-ASK-DUKE.
https://www.hr.duke.edu/pas/
Upcoming Dates and Events
February 17 - Duke vs UNC @Tobacco Rd.
March 2 - JAR Networking Event
March 5 - UNC vs Duke
March 18 - Match Day Celebration
April 29 -Charity Auction
Useful links
GME Mistreatment Reporting Site
https://intranet.dm.duke.edu/influenza/SitePages/Home.aspx
http://duke.exitcareoncall.com/
Main Internal Medicine Residency website
Main Curriculum website
Department of Medicine
Confidential Comment Line Note: ALL submissions are strictly confidential unless you chose to complete the optional section requesting a response
Opportunities
www.bidmc.org/CentersandDepartments/Departments/BIDHC
http://www.careermd.com/employers/latestbulletins.aspx