From the Director

Hope you all enjoyed a rainy weekend! Had a really fun JAR dinner at M Sushi with Jenny Van Kirk, Lakshmi Krishnan, Mike Dorry, Taylor Bazemore and Drew DeMaio. Look for the pic of Taylor’s “State of NC” shaped grilled octopus!
Thanks to all who came out to play and support the housestaff and faculty at Cameron Indoor. Game was called early after an injury, but the faculty was starting to get winded and the residents were poised for a big comeback, for sure! We moved right from the game to the AMAZING Charity Auction! Many many thanks to our planning committee Jessie Seidelman, Andrea Sitlinger (co-chairs), as well as Maggie Moses, Sarah Nouri, Maggie Infeld and Liz Gilbert, as well as our unstoppable office team of Jen Averitt, Madi Smith, Tia Williams and Lynsey Michnowicz. Special thanks to Ryan Jesse, Nick Foster and Adva Eisenberg for helping set up and to Nick being the DJ. And, of course, our wonderful emcee Dr. G! Final totals to follow, as well as special thanks to all faculty who donated (the entire list is pending, so we don’t want to leave anyone out!)
More activities to come this week and into next. Today our Learning Health System Training Program residents present to Dr. Washington and Dr. Owens. Representing the medicine residency are Andrea Sitlinger and Matt Atkins. Also presenting are Armando Bedoya, Meredith Clement and Rebecca Sadun! This is our third year of the program — any questions, please see me, as applications are being posted for next year!
Kudos this week from Bassem Matta to Andy Mumm for amazing work with a life-saving diagnosis at the Lincoln Clinic. Kudos also this week to our amazing ACRS Bassem “1010 is fun” Matta, Adva “You see a problem, yo! I’ll solve it” Eisenberg, and Steph “Making Morning Report Great, even at 7:15” Giattino. Welcome to our new ACRS Andrea Sitlinger, Kristen Glisinski and LiWen Huang. Other kudos to Jackie Bolwell from Liz Hankolari and a patient who said that Jackie was “the bright spot of her very long hospital stay”. Also to the team of Jenn Rymer, Ashley Bock and Jackie Bolwell from another patient who dropped off some nice books for the team to thank them for great care.
This week’s pubmed from the program goes to David Kopin for his article in PLosOne! PLoS One. 2016 Mar 3;11(3):e0150606. doi: 10.1371/journal.pone.0150606. eCollection 2016. A Protocol for the Comprehensive Flow Cytometric Analysis of Immune Cells in Normal and Inflamed Murine Non-Lymphoid Tissues. Yu YR1, O'Koren EG2, Hotten DF3, Kan MJ2, Kopin D4, Nelson ER5, Que L1, Gunn MD3.
Have a great week!
Aimee

What Did I Read This Week?

Submitted by Lynn Bowlby, MD
JAMA. 2016;315(15):1624-1645 4/19/16
Special Communication: CDC Guidelines for Prescribing Opioids for Chronic Pain—United States, 2016
All of you who know the DOC and our policies regarding opioids knew that you would see this discussed here!
This very important topic is gaining increasing momentum and I was surprised, and pleased, to see the CDC weigh in with these easy to use guidelines. The increased use of opioids for chronic non-cancer pain when the focus was on providing treatment for pain in the early 2000s has had some unintended consequences. It is very helpful to have these guidelines and national standards.
To summarize the JAMA/CDC guidelines—
Chronic non cancer pain is very common in the US—11.2% of the adult population.
Evidence supports the short term efficacy of opiates, 12 weeks or less. Few studies look at pain > 3 mos and outcomes > 1 yr.
Opioids have serious risks—1999-2014 , 165, 000 people died, and in 2013, 1. 9 million abused or dependent on opioids.
These guidelines are meant for primary care physicians dealing with chronic pain, > 3 mos, and not palliative, end of life or active cancer pain.
The guidelines were developed with the GRADE method, examining the quality of evidence and getting stakeholder input from multiple partners, agencies and experts.
With a systematic review, esp. looking for evidence of long-term benefit, 5 KQ (Key Questions) were developed, each with sub-questions.
Some highlights from the KQs:
Most placebo controlled trials were < 6 weeks.
Long term opioid therapy was often associated with problematic patterns of opioid use, leading to clinically significant impairment or distress aka addiction, opioid abuse and dependence.
Prevalence of this 3-26% in primary care settings.
Increase risk of misuse with history of Sub Abuse, younger , major depression and use of psychotropic meds.
Initiation of opioids with Long acting (LA) meds had higher risk of nonfatal OD, esp in first 2 weeks.
Accuracy of the risk assess. Tools ie. The ORT , is very limited.
Opioids started for early acute issue ie. Back pain, much more likely to lead to long term use.
Non pharm and nonopioid meds with evidence for effectiveness included CBT, exercise therapy, acetaminophen, NSAIDs, gabapentin and preglablin.
Opioid related OD risk is dose dependent, with dosages > 50 MME (Morphine mg equiv)/ day
Inc. risk with methadone, co-prescription of opioids and benzos, OSA, renal or hepatic impairment, older and pregnancy.
Some risk reduction strategies, ie. State drug monitoring program and UDSs may be helpful.
12 Recommendations—
No evidence shows a long-term benefit of opioids in pain and function vs. no opioids
Possible harms shown in extensive evidence
Some benefits of nonpharm and non opoiods with less harm, also with extensive evidence
Opioids should not be considered first line for chronic pain.
Determine how effectiveness will be monitored and goals est. with pts.
Improvement in function should be the primary goal.
Discuss storage and risk of having opiods at home, and risks of sharing
If prescribing, start with short acting, and use methadone only if familiar with the unique risk profile (we are and do at the DOC)
Use lowest effective dose.
Continually evaluate the benefits and risks and review with pts how you will help them off the opioids if needed.
Review the state data base, and consider offering naloxone .
It seems that we moved from never using opioids for chronic non-cancer pain, to over-using them.
Now the challenge is to find the balance and help our patients with chronic pain, while keeping them safe.
QI CORNER
This feature will return next week
CLINIC CORNER

Hi DOC residents!
Hope you are all doing well!
A few, and serious, items—
1. Staffing—you will see temp staff to cover the openings in clinic staff.They are very skilled, but don’t know us, nor our patients well. The Nurse manager job, Gina Green’s position is still open, we are working hard to fill it.
2. Suicide-
We recently had a suicide attempt by a pt, who had seen us recently , depressed, with thoughts of death but denied SI.
She had notified her husband who found her hanging and got her to the ED.
The CDC recently released their national statistics showing an increase in suicide in this country.
Jan and I talked at length—
Here are the things to know—
We have a lot of pts with passive or chronic SI—these are very challenging. They are at greatest risk as Jan notes below with an acute major stressor or if they have had a prior suicide attempt.
For any pt with concern about SI, Jan would be the point person to see those pts, NOT Ashley or Joy.
Page covering SW or interrupt Jan for this safely issue as needed.
Pts CANNOT refuse to talk with Jan if concern is suicide.
Below is what Jan uses in her evaluation.
Things that I think would bump up the need for a consult include prior attempt and acute stressor.
This is the SAFE-T suicide risk assessment (Suicide Assessment Five-step Evaluation and Triage). It is my preferred tool, although there are many.
1. RISK FACTORS
Suicidal behavior: history of prior suicide attempts, aborted suicide attempts or self-injurious behavior
Current/past psychiatric disorders: especially mood disorders, psychotic disorders, alcohol/substance abuse, ADHD, TBI, PTSD, Cluster B personality disorders, conduct disorders (antisocial behavior, aggression, impulsivity). Co-morbidity and recent onset of illness increase risk
Key symptoms: anhedonia, impulsivity, hopelessness, anxiety/panic, insomnia, command hallucinations
Family history: of suicide, attempts or Axis 1 psychiatric disorders requiring hospitalization
Precipitants/Stressors/Interpersonal: triggering events leading to humiliation, shame or despair (e.g., loss of relationship, financial or health status—real or anticipated). Ongoing medical illness (esp. CNS disorders, pain). Intoxication. Family turmoil/chaos. History of physical or sexual abuse. Social isolation.
Change in treatment: discharge from psychiatric hospital, provider or treatment change
Access to firearms
2. PROTECTIVE FACTORS
Internal: ability to cope with stress, religious beliefs, frustration tolerance
External: responsibility to children or beloved pets, positive therapeutic relationships, social supports
3. SUICIDE INQUIRY Specific questioning about thoughts, plans, behaviors, intent
Ideation: frequency, intensity, duration--in last 48 hours, past month and worst ever
Plan: timing, location, lethality, availability, preparatory acts
Behaviors: past attempts, aborted attempts, rehearsals (tying noose, loading gun), vs. non-suicidal self-injurious actions
Intent: extent to which the patient (1) expects to carry out the plan and (2) believes the plan/act to be lethal vs. self-injurious; Explore ambivalence: reasons to die vs. reasons to live
4. RISK LEVEL/INTERVENTION
Assessment of risk level is based on clinical judgment, after completing steps 1-3
Reassess as patient or environmental circumstances change
RISK LEVEL RISK / PROTECTIVE FACTOR / SUICIDALITY POSSIBLE / INTERVENTIONS
High Psychiatric disorders with severe symptoms, or acute precipitating event; protective factors not relevant Potentially lethal suicide attempt or persistent ideation with strong intent or suicide rehearsal
Admission generally indicated unless a significant change reduces risk. Suicide precautions
Moderate Multiple risk factors, few protective factors Suicidal ideation with plan, but no intent or behavior Admission may be necessary depending on risk factors. Develop crisis plan. Give emergency/crisis numbers
Low Modifiable risk factors, strong protective factors Thoughts of death, no plan, intent or behavior Outpatient referral, symptom reduction. Give emergency/crisis numbers
5. DOCUMENT Risk level and rationale; treatment plan to address/reduce current risk (e.g., setting, medication, psychotherapy, E.C.T., contact with significant others, consultation); firearm instructions, if relevant; follow up plan..
3. SARs—use smart phrase from Jonathon Hansen , .dochandoff for your more complex handoffs, and a warm handoff for your 10 or so most complex.
Say goodbye to your patients, it is hard, but the right thing, and help them transition to their new doctor.
4. Ashley and Joy—new Beh Health counselors—refer for mental illness as well as lifestyle issues, smoking, obesity.
5. Refill meds when pt in clinic, and check your inbasket…attendings are helping with calls/refills etc.
6. DOC Fund—thanks for the great Auction Friday night, so , so much work to put that together!
7. Town Hall for Continuity Clinics – this past week, thanks to all who attended!
Natasha Cunningham leaves to move to CA June 17, her wedding was yesterday!
Photo in next DOC Clinic corner if she will let us!
8. We are having all of you listed on line as available PCPs for patients searching on line…you will be asked to fill out some on line info, please complete and let me know if there are any questions!
If you have needs for patients, and want to use the fund, contact Jan or myself. We have a small amt of cash on site from the fund.
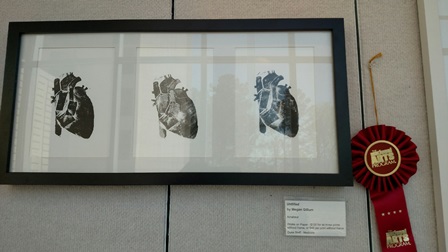
Finally, congratulations to Megan Gillum for her amazing, award winning art work!
Thanks all for your great work!
Lynn and co.
From the Chief Residents
Grand Rounds
Friday, May 6 - Infectious Disease, Ephraim Tsalik
Noon Conference
| Date | Topic | Lecturer | Time | Vendor |
| 5/2/16 |
Cardiac hemodynamics and the Physical Exam |
Thomas Bashore |
2002/12:00 | Domino's |
| 5/3/16 |
Outpatient Management of CHF/Zubin Eapen |
2002/12:00 | Nosh | |
| 5/4/16 |
MKSAP Cards |
|
12:00/MedRes | China King |
| 5/5/16 |
IM-ED Combined Conference: Ultrasound / G-Briefing |
Bri Steele / Dr. G |
2001/MedRes |
Subway |
| 5/6/16 |
Chair's Conference |
Chiefs | 12:00/2002 | Jason's Deli |
From the Residency Office
Stead Sponsored Event
STEAD Mentoring event this FRIDAY, May 6th from 5-7pm
Faculty Discussants:
Lisa Criscione-Schreiber, MD
Kevin Thomas, MD
Heather Whitson, MD
Please come join us in the faculty lounge for drinks, food and great conversation.
Hope to see you there!
Attention DOC Residents and Prelim Interns
I’m very excited to share information about our expanded behavioral health services at DOC. In addition to having Jan onsite to provide targeted counseling, we have hired 2 Master’s-level behavioral health consultants who are available to see patients immediately after your visit or by appointment. All 3 can see patients up to 6 times and are true behavioral health generalists helping with issues such as depression, anxiety, PTSD, substance abuse, bereavement, etc. They can also help patients with wellness behaviors such as exercising consistently, taking meds, eating better, improving sleep etc. Joy Long and Ashley Cyr are our new folks and Jan Dillard remains enthusiastic about serving our patients. Please take 5-10 minutes and look at the attached PowerPoint slide deck entitled “Resident Info PPT” (attached as a PDF at the end of this post) put together by Krupa, the grad student who has been helping with our project. There is no cost to the patient for any of these services. Our behavioral health team will communicate with you directly and in Maestro.
In addition, we have begun screening all patients for depression and will soon expand the range of social and behavioral issues for which we screen.
Larry Greenblatt
Office Hours for Dr. Zaas
Dr. Zaas will have the following office hours. Please feel free to stop by during these times and of course always feel free to reach out to her office to set up a meeting outside of these times if needed!
Monday - 3:00 p.m. to 4:00 p.m.
Thursday 10:00 a.m. to 11:00 a.m.
General Internal Medicine Career Night
General Internal Medicine Career Night
Interested in a career in General Internal Medicine?
Thinking about primary care medicine, Gen Med fellowship or hospitalist medicine?
Envision working in academics, research, Quality Improvement
or a combination?
Come to Gen Med Career Night
Tuesday May 3, 2016
6:30-8:30pm
Gen Med Resident Library
Dinner from Nosh
Come ask questions for our panelists about their path and journey:
Kevin Shah, Claire Kappa, Sharon Rubin, David Edelman, Sonal Patel, Lance Teagen, David Gallagher and Daniella Zipkin
Please RSVP to Sharon.rubin@dm.duke.edu by May 2, 2016
Charity Auction 2016 - A HUGE Success
Thank everyone who came out to the event and everyone who donated! First, a special thanks to Dr. Zaas for her incredible suppprt and to and Dr. G for his hosting! I would also like to thank Maggie Infeld and Liz Gilbert for for their incredible work getting all of the donations from sponsors; Jen Averitt, Tia, Madi, and Lynsey for helping us all year to get the venue and the rest of the logistics squared away; Adva Eisenberg, Ryan Jessee and Rowan Averitt for helping with set-up; Gena and Nick Foster for providing the wonderful entertainment; and last but not least Andrea Sitlinger for being such an incredible co-chair. She worked tirelessly at this event and made it look easy despite having a newborn and being on Duke Gen Med.
Thank you all!
Jessie Seidelman, Charity Auction 2016 Co-Chair
LiveSafe Mobile App
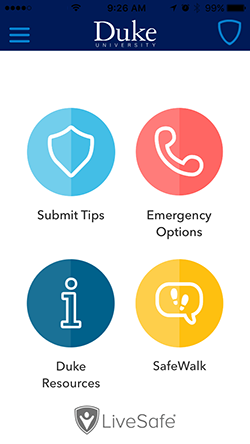
Duke is introducing a new mobile app called LiveSafe to put a powerful safety tool in the hands of the Duke community.
The app, available as a free download from Apple and Android app stores, enables smartphone users to submit real-time tips to Duke Police, virtually “SafeWalk” friends and family while traveling, place emergency calls, and access important resources for support.
You can find more information, including instructions on how to download the free app, on the DukeALERT website: http://emergency.duke.edu/notified/livesafe.
Opportunities for Wellness
Feeling down? Need to talk to someone?
All trainees at Duke have FREE access to Personal Assistance Services (PAS), which is the faculty/employee assistance program of Duke University. The staff of licensed professionals offer confidential assessment, short-term counseling, and referrals to help resolve a range of personal, work, and family problems. PAS services are available free of charge to Duke faculty and staff, and their immediate family members. An appointment to meet with a PAS counselor may be arranged by calling the PAS office at 919-416-1PAS (919-416-1727), Monday through Friday between 8:00 A.M. and 5:00 P.M. For assistance after hours, residents and fellows can call the Blood and Body Fluid Hotline (115 inside DUH, 919-684-1115 outside) for referral to behavioral health resources. Another resource is Duke Outpatient Psychiatry Referrals at (919) 684-0100 or 1-888-ASK-DUKE.
https://www.hr.duke.edu/pas/
Upcoming Dates and Events
May 14 - Spring Picnic
May 20 - Resident Research Grand Rounds
May 20-21 - 2nd Annual Family Weekend
May 31 - Rising JAR Retreat
June 1 - Rising SAR Retreat
June 4 - SAR Dinner
Useful links
GME Mistreatment Reporting Site
https://intranet.dm.duke.edu/influenza/SitePages/Home.aspx
http://duke.exitcareoncall.com/
Main Internal Medicine Residency website
Main Curriculum website
Department of Medicine
Confidential Comment Line Note: ALL submissions are strictly confidential unless you chose to complete the optional section requesting a response
Opportunities
www.bidmc.org/CentersandDepartments/Departments/BIDHC
http://www.careermd.com/employers/latestbulletins.aspx