From the Director

We have had a lot to celebrate in the past week! Congratulations to Eric Black-Maier and Allison Canter on their wedding, Adam Banks and Lisa and Sarah Goldstein and Marc Samsky on their weddings this past weekend! Also welcome to the Duke family to Klara Bazemore, born to proud parents Taylor and Jillian, as well as congratulations to proud parents Stephen and Erin Bergin on the birth of their son Benjamin!
This week, we are hosting our first rising JAR and rising SAR retreats. Much thanks again to all who arranged coverage and who are covering. We are looking forward to some great discussion and class activities. Saturday night is the night that we celebrate our graduating SARs with the SAR dinner. Also thanks to all who are covering so that all SARs can attend.
Please complete your iCOMPARE survey if you receive one from the iCOMPARE study team. The programs with the top completion rates get FAT CASH. Which we would use for RESIDENT SOCIAL EVENTS. I do not get to see who fills out the survey, so I can only encourage participation to all. Also, have some fun participating in the country-wide MKSAP challenge, with cases emailed to you each day.
Kudos this week to Caroline Sloan for earning a Gold Star from a patient compliment, as well as to Brian Sullivan from Josh Lee and the gen med team for being a fantastic SAR last month on gen med. Kudos also to Kara Wegermann and John Yeatts from jenn Rymer! A huge congratulations as well to Lindsay Boole on her fantastic Grand Rounds. We are looking forward to hearing from Chris Hostler on Friday.
Don’t forget that fellowship ERAS opens on June 9th if you are applying! Once you get your ERAS token, you can assign your LOR writers and they will be able to upload letters. Any questions, please check in with Bill and me.
Lincoln volunteer opportunity sign up closes on JUNE 3rd!
This week’s pubmed from the program goes to Bhavana Singh for her article published earlier this year with mentor April Salama. B. Singh, A. Salama. Updates in Therapy for Advanced Melanoma. Cancers (Basel). 2016 Jan 15;8(1). pii: E17. doi: 10.3390/cancers8010017.
Have a great week!
Aimee




What Did I Read This Week?
Denson JL, Jensen A, Saag H, Wang B, Fang Y, Horwitz L, Evans L, Sherman S. Increased Mortality Associated With Resident Handoff in A Multi-Center Cohort. Poster session presented at the American Thoracic Society International Meeting; 2016 May 16; San Francisco, CA.
http://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2016.193.1_MeetingAbstracts.A7568
What if I told you your patients are 20% more likely to die if their hospital stay includes a block transition?
I read this abstract from ATS because one of the authors is a CRQS and I had heard about it from him. The headline is getting a lot of attention though—it came across in one of my journal watch emails this week (http://www.medpagetoday.com/MeetingCoverage/ATS/57991). You’ll see why.
They did a retrospective cohort study using data from 10 academic VAs, and they had access to the block schedules at each. The “exposure” was being admitted before a block transition and then discharged within 7 days after a block transition. They had data from 230,701 discharges, gleaned from the VA’s huge Clinical Data Warehouse.
30-day mortality was 20% higher in patients whose intern had changed over within 7 days prior to their discharge, controlling for age, sex, race, ethnicity, length of stay, calendar month, and comorbidity index. It was 15% higher in patients whose resident had changed over, and 10% higher when both intern and resident had changed over (p values all very significant). The risk persisted to 90-day mortality, with 17%, 14%, and 9% higher mortality, respectively.
Interesting that the intern handoff has the strongest effect, stronger even than the intern+resident handoff. Maybe block-to-block handoff is a skill that improves with training; or maybe JARs/SARs know enough to be afraid and just exercise more caution when making one of these transitions. (Do you think you worried more about these handoffs the farther along you got? I did.)
But 20%! If there were a biological exposure or behavior that we knew raised 30-day mortality by 20%, we’d be aggressively treating or eliminating that exposure. (We anticoagulate in afib for a heck of a lot less, right Jenn?) But residents gotta rotate… So what to do?
Some institutions are setting the expectation of a “warm handoff” to transfer information. That’s something that only works in a x+y scheduling system: the oncoming intern/resident comes in the Sunday afternoon or evening before they start the block and get bedside handoff from their offgoing counterpart. Some of you probably already do this. It makes sense—and we may see a future study from these authors determining whether it helps.
QI CORNER
I want to congratulate Lindsay Boole for her outstanding grand rounds presentation last week!! If you didn't see it live, I would definitely encourage you to watch it from the department website. She shared her story of trying to improve the VA performance for a specific hospital acquired infection metric now renamed VAEs (ventilator associated events). The talk was perfectly delivered and filled with cornerstone QI tools.
On another note, we will be closing out the JAR & SAR sharepoint QI project on "Goals of Care in clinic" at the end of June. PLEASE finish up your second chart review so I won't have to hound you:) We welcome your input about next years QI project - please feel free to email Lish your suggestions.
Clinic Corner
Hey everyone!
“LPS” Continuity Clinic Survey is out!!
I realize you are all being heavily surveyed in these closing months of the year – thank you for also filling out the LPS, Learner Perceptions Survey, now in MebHub. We need to hear your thoughts on your CONTINUITY sites to keep working on improving your experience. Thanks so much!
Clinic orientation for the new interns
Will be held on June 29th from 3-5 PM at each clinic site – if you are there that day, talk to your clinic lead about stopping in to say hello!
ACLT Updates
The ACLT successfully advocated on Capitol Hill around the opioid crisis, asking legislative staff for a national controlled substances reporting database and for funding for non-opioid pain management alternatives in the current bills. There is strong bipartisan support for opioid legislation but the trick is putting appropriations (i.e. $$$) behind it!! The group also met with leadership from the AAMC, the National Academy of Medicine (formerly Institute of Medicine), and Health and Human Services.
From the Chief Residents
Grand Rounds
Friday, June 3 - VA Chief: Dr. Chris Hostler
Noon Conference
| Date | Topic | Lecturer | Time | Vendor | |
| 5/30/16 |
MEMORIAL DAY - NO CONFERENCE |
|
12:00 | ||
| 5/31/16 |
Perioperative Management of Diabetes |
Tracy Setji |
Nosh |
||
| 6/1/16 |
Medical Problems of Pregnancy |
Lynn Bowlby | 12:00 | China King | |
| 6/2/16 |
IM-ED Combined Conference: Cardiogenic Shock |
Adam Devore | 12:00 | Subway | |
| 6/3/16 |
Chair's Conference |
12:00 | Jason's Deli |
From the Residency Office
GME Survey
Dear GME Residents and Fellows:
You should have all received two important surveys over the past few weeks, and we need your input as we continue to work to enhance the learning environment.
The first is our annual housestaff survey. This survey came from docr.survey@dm.duke.edu. This survey represents your opportunity to anonymously assess the learning environment and provide feedback about your experiences here at Duke. These results are used every year to make improvements and we need your input. If you cannot find your link or have any questions, please contact Dr. Kuhn at catherine.kuhn@duke.edu.
The second survey is the SCORE safety culture survey. This survey came from surveys@safeandreliablecare.com. This survey provides the health system with information about our safety practices and culture, and your input is essential.
We look forward to hearing your input and please let us know if you have any questions or concerns.
David A. Turner, MD
Associate Director, Graduate Medical Education
Duke University Hospital and Health System
Associate Professor, Department of Pediatrics
Division of Pediatric Critical Care
Duke Children’s Hospital
Hospital Medicine Interest Night
Graduating Residents in 2017
Monday June 13, 2016
5:30-7:00pm
Nosh Café @ Trent Semans Building
Dinner Provided By Nosh
Come to discuss Hospitalist Opportunities with our Hospital Medicine Leadership
Attendees: David Gallagher, Noppon Setji, Lalit Verma, James Soldin, Cara O’Brien, Adam Wachter, Jonathan Bae
Medical Improv Workshop
I’m writing to invite you to take part in a new learning offering for members of the Duke and UNC Health Sciences. It’s one of the first Medical Improv Workshop being offered in the Triangle area. And it’s free!
Medical Improv is quickly gaining popularity as an innovative approach to teaching principles that are at the heart of patient centered care: Deep listening, collaboration and seeing things from other’s point of view. Medical Improv can help teach skills that will make you more present and aware during high stakes conversations with patients and colleagues. If you find yourself feeling overwhelmed by everything that’s coming at you during your time with patients, these skills can help things slow down a little so you can prioritize what’s most important and make better decisions.
This 3 hour pilot workshop is free to all Triangle health professions students and clinicians on a first-come-first-served basis. The workshop will be capped at 15 students for more individualized attention. No observers will be allowed in these sessions. Everyone will be expected to participate. The sessions will not be recorded in any way and no grades will be given. The goal is to create a safe environment where people can play and speak freely.
These sessions will be led by Dan Sipp, a trainer for the Clinical Skills Program at Duke Medical School. Dan has taught improvisation in Chicago and the Triangle for over 20 years. He’s trained with the creator of Medical Improv, Katie Watson of Northwestern University’s Feinberg School of Medicine*, and they have collaborated on projects for the University of Indiana School of Nursing. Dan is very excited to bring these sessions to medical learners in the Triangle. Duke Faculty members from the School of Medicine, Graduate Medical Education, The School of Physical Therapy and The Physician Assistant Program will be co-facilitating these and upcoming sessions.
You’re invited to register this free workshop!
Saturday, June 11th 10 a.m. to 1 p.m. @ Trent Semans Center for Health Education, 6th floor
To reserve your spot in the next Medical Improv Workshop please email Dan. Once he receives your email he’ll follow up with a confirmation of your spot, directions to the site and more information about the day.
Remember space is limited to 15 participants per session. We want to see you there. So sign up soon! You are also free to forward this email onto friends or colleagues who you feel might be interested in this innovative training session.
Sincerely,
Dan Sipp
919-681-8681
Office Hours for Dr. Zaas
Dr. Zaas will have the following office hours. Please feel free to stop by during these times and of course always feel free to reach out to her office to set up a meeting outside of these times if needed!
Monday - 3:00 p.m. to 4:00 p.m.
Thursday 10:00 a.m. to 11:00 a.m.
LiveSafe Mobile App
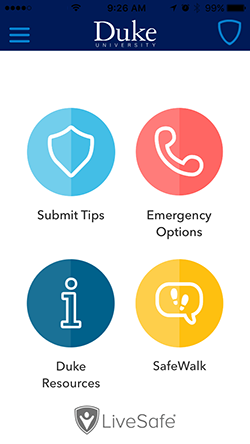
Duke is introducing a new mobile app called LiveSafe to put a powerful safety tool in the hands of the Duke community.
The app, available as a free download from Apple and Android app stores, enables smartphone users to submit real-time tips to Duke Police, virtually “SafeWalk” friends and family while traveling, place emergency calls, and access important resources for support.
You can find more information, including instructions on how to download the free app, on the DukeALERT website: http://emergency.duke.edu/notified/livesafe.
Opportunities for Wellness
Feeling down? Need to talk to someone?
All trainees at Duke have FREE access to Personal Assistance Services (PAS), which is the faculty/employee assistance program of Duke University. The staff of licensed professionals offer confidential assessment, short-term counseling, and referrals to help resolve a range of personal, work, and family problems. PAS services are available free of charge to Duke faculty and staff, and their immediate family members. An appointment to meet with a PAS counselor may be arranged by calling the PAS office at 919-416-1PAS (919-416-1727), Monday through Friday between 8:00 A.M. and 5:00 P.M. For assistance after hours, residents and fellows can call the Blood and Body Fluid Hotline (115 inside DUH, 919-684-1115 outside) for referral to behavioral health resources. Another resource is Duke Outpatient Psychiatry Referrals at (919) 684-0100 or 1-888-ASK-DUKE.
https://www.hr.duke.edu/pas/
Upcoming Dates and Events
May 31 - Rising JAR Retreat
June 1 - Rising SAR Retreat
June 4 - SAR Dinner
June 5th, 11am - First Annual Spike and Swim
June 24 - 30th - Intern Orientation Week
Useful links
GME Mistreatment Reporting Site
https://intranet.dm.duke.edu/influenza/SitePages/Home.aspx
http://duke.exitcareoncall.com/
Main Internal Medicine Residency website
Main Curriculum website
Department of Medicine
Confidential Comment Line Note: ALL submissions are strictly confidential unless you chose to complete the optional section requesting a response
Opportunities
https://www.phs.wakehealth.edu/public/edu.cfm
www.bidmc.org/CentersandDepartments/Departments/BIDHC
http://www.careermd.com/employers/latestbulletins.aspx