For the Director

As some of you may know, Dr. Zaas suffered a tremendous personal loss this past weekend when her father, Dr. Morton Kirsch, passed away. Please keep Dr. Zaas and her family in your thoughts and prayers during this difficult time. Look for her return to this post very soon!
All families face challenges and adversities that life can throw at us - our family is no different. Thank you to everyone who has offered their support these past few weeks. The love and kindness that everyone has shown to us and each other has been inspiring. As we all continue to deal with our grief and begin the healing process, please remember that there are resources (included at the end of this post) available to help you. In addition, Dr. Galanos will be hosting a special d-brief for Noon Conference on 9/24/15 and the program will be hosting informal support-group lunches for those who would like to attend - information on those will be forthcoming via email. As always, the MedRes office is here if you need anything.
#dukefamily
Best,
Jen
What did I read this week?

Submitted by Dr. Lynn Bowlby
Nathan, D; Diabetes Advances in Diagnosis and Treatment. JAMA. 2015;314 (10):1052-1062.
2 articles this week caught my eye in the 2 paper journals I receive at home. With the large number of patients with DM we care for every week at the DOC reviews on this topic are welcome. Dr Nathan, the author, leads the MGH Diabetes Center.
Diabetes is one the major public health challenges world wide today. While Type 1 DM has been slowly increasing in indidence, it still is less than 5% of the cases of DM in the US. World wide, > 350 million people have Type 2 DM. DM has very specific complications, and is the #1 cause of vision loss, ESRD, and amputaions. The risk of CVD is increased x5. The economic burden of both DM and pre-DM is estimated to be $322 billion/annually.
Advances in Diagnosis:
Historically the metabolic disturbances rely on blood glucose level measurement. The enzymatic methods haven’t changed but the devices have become smaller, faster and more accurate. The newest method is continuous glucose monitoring with an indwelling catheter in the subcutis and changed every 3-7 days. A1C has been used to measure chroic levels of glycemia for 30 years. The are now standardized and reliable. A1C has now been added to the diagnostic strategies due to this and the knowledge that chronic glycemia is related to compications just like glucose levels. Glucose levels and A1C reflect different metabolic issues. The recommended populations to screen have not changed in > 10 years: > 45, BMI > 25, inactive , gestational DM, HTN, hyperlipidemia or CVD.
Type 1 and 2 DM are polygenetic, with almost 100 genes involved in Type 2 DM. Fewer genes with Type 1 DM, most are from autoimmunity. The environmental factors work with the genetic issues for Type 2 DM. Genotyping may help to identify subtypes of Type 2 DM, and individualize the treatment.
Advances in Prevention:
Immune manipulation to prevent Type 1 DM in the ENDIT and DPT-1 studies was attempted, but no change in incidence of Type 1 DM was found. For Type 2 DM , DPP showed lifestyle interventions for obesity and sedentary lifestyle reduced DM by 58%. Metformin is the only other strategy for prevention, especially for those < 60 with a BMI of > 35.
For the first time in 30 years the incidence of Type 2 DM seems to be decreasing in the US.
Advances in Management:
Goal is long term glycemic control. Long lasting effects, termed metabolic memory, persist beyond the period of glycemic control. Data for CVD risk reduction less clear with Type 2 DM, 2 recent studies show reduction of 15-17 % in CVD risk with intensive glycemic therapy. Type 1 DM is more complex , and often relies on devices, so specialty management much more common. Basal insulin is meant to provide insulin for overnight use when pts are not eating. NPH or glargine are generally used. Glargine has minimally lower A1C (<0.1%) data and slightly less hypoglycemia as compared to NPH. 2 new very long acting insulins, degludec and U-300 glargine are now available. The high costs of all of these, but NPH, are barriers to their use.
Preprandial insulin has similar data with the newer rapid acting insulins only marginally better (0.09%) in lowering A1C than the older and less expensive regular insulin.
Insulin pumps with marginally lower A1C levels.
Inhaled insulins have been released again. The first release was 2006, then removed from the market a year later due to poor sales.
Continuous glucose monitoring is available, especially with insulin pumps, but it is not clear if glycemic control is improved.
For Type 1 DM, pancreatic or islet cell transplants are available. There is limited available organs. Islet cell transplant is still experimental.
Type 2 DM
The number of medications has more than tripled, with 1-5 drugs per class.
There is very little data to guide which medications to choose. Patients with Type 2 DM are generally treated similarly, yet there is increasing knowledge that it is a very heterogenous disease. The GRADE study is currently ongoing, a comparative effectiveness study, with medications added to metformin. Until we have this data, we choose medications with very limited data.
Aggressive therapy, usually with insulin, can improve insulin secretion and allow for a repite from medications for several years. The first medication used , after lifestyle advice, is metformin. There is little evidence for this to be our first choice, and in other countries , other medications are dominant. The choice of the second medication is even less clear, until the GRADE study results are available. The current studies are only 6- 12 months, and the FDA only requires a reduction in A1C of 0.5% for drug approval. Most of the data of glycemic control remains with insulin and the sulfonureas. Risk of hypoglycemia with insulin is much lower with Type 2 DM than with Type 1 DM.
TZDs with increased CVD risk, fluid retention, CHF and bone loss limits their use. GLP-1 agonists also cause weight loss, lower A1C by 1%. DPP-4 inhibitors lower A1C by 0.6-0.8% , weight neutral. The newest medication is SGLT-2 inhibitors, blocks glucose reabsorption in the renal tubules. The are relatively weak, weight neutral, and lower BP. These last 3 medications are expensive, with unclear benefit. Even well insured patients can have high co-pays with the more expensive medications. There are exciting new developments in the management of DM. This very important chronic illness has new hope for better management and diagnosis.
QI CORNER
Last week, the Patient Safety and Quality Council (PSQC) met and selected several exciting projects for this year. If you were not able to make the meeting but are interested in getting involved in QI, please email me so I can include you on our emails as we get started with this work!
Also, another plug for the Making Wise Choices Easier competition. Most of our PSQC residents are forming into teams to put proposals together, so get in touch with me if you want to get involved. The competition is open to ALL housestaff, not just PSQC members, and I'm happy to help you work through ideas if you want to put together a proposal together outside of that committee. The deadline for submissions is Oct 19th! See the pdf flier (attached, or on the med res bulletin board) for submission details.
Please join us THIS WEDNESDAY at noon conference, where we will be introducing your ambulatory Sharepoint project for this year. Dr. Trig Brown from Palliative Care will be presenting on the topic, which is goals of care conversations in the outpatient setting. All JARs and SARs will complete the Sharepoint assignment, so this is your chance to get up to speed on what it is all about.
Then at Thursday's noon conference, we have a QI talk on healthcare waste, costs and over-ordering of tests from hospitalist Dr. Dan Kaplan.
I look forward to seeing all of you at these great talks. Have a fantastic week!
CLINIC CORNER

Dr. Sharon Rubin, Pickett Road Clinic
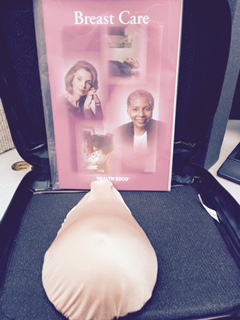
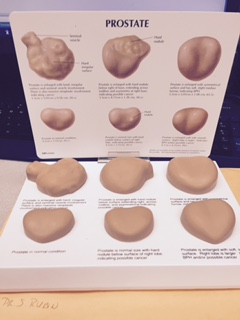
We have some new models at the clinic (see the pictures). You will need to use some pressure to examine the breast model and test your tactile skills with the prostate model.
Dr. Metz is our pan optic champion! If you need help and instruction the pan optic will be located at her desk. If you have a patient you are worried about please come try to use the pan optic. Rooming nurses will be placing orders that are due for annual patient visits and associating with visit diagnosis. This is a part of the Transforming Primary Care lead by Dr. Jennifer King. Rooming nurses are calling patients the day before to confirm the appointment and some medicine reconciliation
Join us for the American Heart Association Heart Walk!
Pickett Road Heart Walk Team! Come Sunday, September 27, 2015 Festivities begin at 12:30pm
Walk begins at 2:00 pm - See more at: http://heartwalk.kintera.org/faf/emailCenter/email.asp?ievent=1125186&lis=0&kntae1125186=B3BB809EEAA64776863B3BE9C98D8252#sthash.8lzfCeHr.dpuf
This is our web site http://heartwalk.kintera.org/trianglenc/pickettroad
From the Chief Residents
Grand Rounds
Friday, September 18 - Dr. Kevin Harrison, Cardiology
Noon Conference
| Date | Topic | Lecturer | Time | Vendor |
| 9/14/15 | SAR Emergency Series: Acute Abdominal Pain |
Alan Erdman |
Domino's | |
| 9/15/15 | MED-PEDS Combined: Contraception/STI |
Beverly Gray |
12:00 | Chick-Fil-A |
| 9/16/15 | QI conference: Sharepoint 2015-16 Discussing goals of care in the clinic |
Trig Brown |
12:00 | China King |
| 9/17/15 | QI Patient Safety Noon Conference- HVCC |
Dan Kaplan |
12:00 | Subway |
| 9/18/15 | Chair's Conference | Chiefs | 12:00 | Firehouse |
From the Residency Office
BLS Blitz - November 2015
Just a reminder that the bi-annual BLS Blitz is coming up in November. The flier posted at the end of this blog has the dates. REMEMBER - Duke only holds BLS classes during the November and March blitz each yer, so if your BLS is expiring before March, PLEASE sign up for one of the dates in November!!
Global Health-Internal Medicine Residency Program Recruiting Eligible Candidates
Internal Medicine Residents who have successfully completed PGY1 are eligible to apply for the Duke Global Health Residency, an extended residency that leads to a Master of Science in Global Health and a total of nine months providing clinical care and conducting mentored research at a Duke University international partner site.
Please visit our website for an in-depth description of the core curriculum including rotations, global health competencies, and program requirements as well as application instructions:www.dukeglobalhealth.org
Watch current global health resident John Stanifer, MD, discuss his decision to pursue global health training at Duke:
Send all application materials electronically to sarah.brittingham@duke.edu.
Applications accepted on a rolling basis until October 1, 2015. Offers will be made in November.
Now Accepting Applications for Global Health Elective Rotations
The Hubert-Yeargan Center for Global Health (HYC) is now accepting applications for Global Health Elective Rotations for July 2016 and March 2017.
Application is open to Duke Cardiology Fellows (PGY 5 & 6) and Duke residents from the Departments of Medicine and Pediatrics: Internal Medicine (PGY 2); Med-Peds (PGY 3); Med-Psych (PGY 4); Neurology (PGY 2), Pediatrics (PGY 2).
The application is attached and available at http://dukeglobalhealth.org/education-and-training/global-health-electi…;
(For detailed site information, send request to tara.pemble@duke.edu).
Interviews will be held in October. For more information about this opportunity, contact Tara Pemble, Program Coordinator at tara.pemble@duke.edu or 668-8352.
Application Deadline: October 5, 2015
Flu Vaccinations - The Blitz is Coming!
GME will kick off our annual flu vaccination campaign with a 24-hour Duke Medicine Mass Flu Vaccination drill on Thursday, September 17, 2015. Mass vaccination clinics will be available at each of the hospitals and clinics throughout DUHS. Following the drill, we will continue our annual flu vaccination program, during which time we will provide many additional opportunities for you to get vaccinated. A schedule of vaccination clinics will be posted on the employee intranet in early September. This list will be updated throughout the vaccination season. Vaccination is also available at Employee Occupational Health and Wellness (EOHW) during business hours.
Applications for Medical or Religious Exemption should be submitted before Monday, October 12, 2015. This will allow sufficient time for review and for communication of the review decision. Please note: Due to the availability of an egg-free formulation of the flu vaccine, egg allergy is no longer a valid reason for a medical exemption.
If you have questions about the flu vaccine or its availability, please visit the DUHS Influenza Resource Guide or duke.edu/flu, ask your manager or contact EOHW.
Together, we can stop the flu. Thank you for your commitment to keeping our patients, and our community, safe and healthy.
Key points for trainees:
Get this done ASAP.
If you have medical exemption, be sure it shows up on your personal OESO Page—contact EOHW for any questions.
If the flu vaccine is received at any site (including the VA) besides DUH, DRH, or DUKE RALEIGH, you should take a picture of your documentation form (legible name, date, location and lot #) and email it to eohwflu@dm.duke.edu.
Please direct any questions to kathryn.andolsek@duke.edu
Upcoming Dates and Events
October 30 - Recruitment Kick-Off Party
December 12 - DOM Holiday Party
Useful links
https://intranet.dm.duke.edu/influenza/SitePages/Home.aspx
http://duke.exitcareoncall.com/
Main Internal Medicine Residency website
Main Curriculum website
Department of Medicine
Confidential Comment Line Note: ALL submissions are strictly confidential unless you chose to complete the optional section requesting a response
Opportunities
http://www.ad001.info/blasts/CKS/CKS15_05431/CKS15_05431.html