Since 2019, the Durham VA has served as the coordinating center for The Pharmacogenomics Testing for Veterans program (PHASER), an exciting new program that is bringing PGx testing to Veterans across the country.
As personalized medicine becomes more extensively researched and available clinically, Veteran Affairs (VA), the nation’s largest integrated healthcare system across the country, serving and caring for over 9 million Veterans, in its nearly 1,300 health care facilities in the United States, are using pharmacogenomic (PGx) testing to optimize prescriptions using genetic data from patients to reduce adverse side effects and improve medication outcomes.
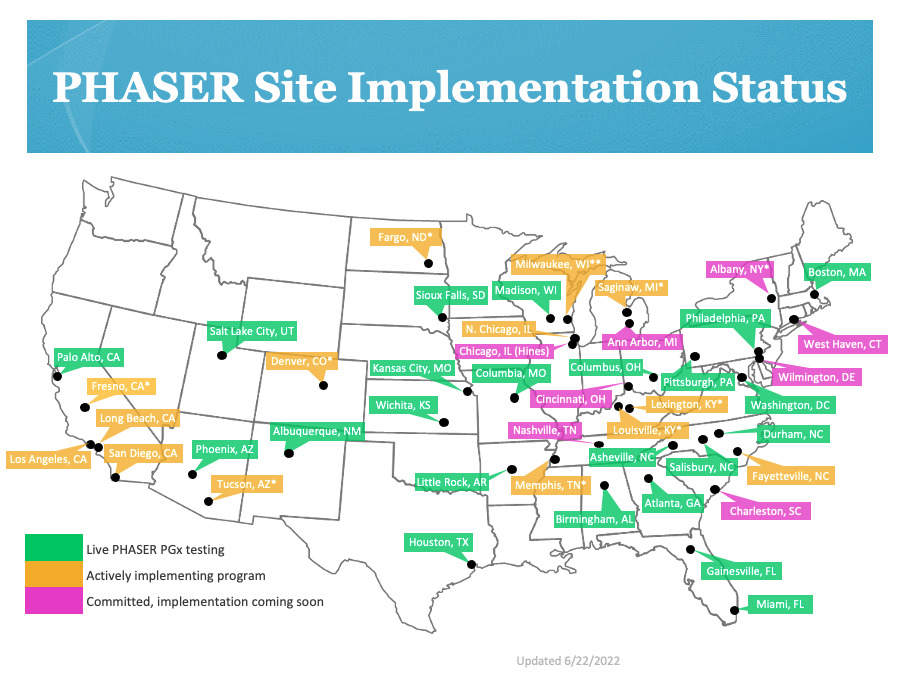
PHASER was launched in 2019 through a collaboration between the VA and Sanford Health Care in Sioux Falls, South Dakota. PHASER utilizes PGx testing, a type of genetic test that assesses a patient's risk of an adverse response or likelihood to respond to a given drug, informing drug selection and dosing, for Veterans. It allows doctors and pharmacists to optimize the dose or type of commonly prescribed medications on their patients. Currently, the program has expanded to approximately 23 VA sites across the nation. Deepak Voora, MD, Associate Professor of Medicine (Cardiology) and faculty at the Duke Center for Applied Genomics & Precision Medicine, was named the founding director of PHASER in 2019.
PHASER has been enrolling patients since its inception and to date has ordered testing in 10,000 Veteran patients nationwide, with the capability to test up to 250,000. PHASER aims to be implemented in 40 to 50 VAs across the country in 2022.
The program provides an end-to-end solution for implementing pharmacogenetic testing at any VA facility for approximately 40 different medications. The process is relatively simple, a single tube of blood is drawn and sent to the lab for testing. The results are returned in about two weeks and entered into the Veteran’s health record, so providers can use this information to optimize prescriptions. PHASER is not only doing the testing but providing the resources to educate patients and providers on who to test and why to test them, as well as guidance on interpreting the test and how to modify prescriptions based on results presented. To help inform providers on how a patient’s genetic test results impact medication prescribing, PHASER has implemented a feature to alert the provider through the patient’s chart, at the point of care of a drug-gene interaction and guide them to ordering a different dose or drug to address the interaction.
For example, when a Veteran is being treated for depression typically, a provider may have to try several different drugs before finding the one that works best for that patient. By using PGx testing, such as PHASER, a provider could identify a drug or dose with lower risk of side effects for the individual patient faster, which, in turn, could create better outcomes and overall better patient satisfaction.
The medications targeted by the panel include anti-depressants, opioids, anti-platelet agents, and cancer agents associated with chemotherapy among others. Providers in primary care and mental health are the two largest groups that have ordered PHASER testing to date.
In addition to implementing PGx testing, VA has recently funded a three-year Quality Improvement (QI) Program to understand the factors associated with using to PGx testing at the health system, provider, and patient levels. Duke investigators collaborating on this QI work include Ryanne Wu, MD, Associate Professor of Medicine (General Internal Medicine) and faculty at the Duke Center for Applied Genomics & Precision Medicine, and Nina Sperber, PhD, Assistant Professor in Population Health Sciences.
“Understanding what factors allow for greater uptake of PGx at some sites and what barriers exist at others is critical to broadening implementation across the VA health system and is what a learning healthcare system is all about,” said Dr. Wu.
Currently PHASER has more than two years left to complete the program. If successful, PHASER will be the largest program of this type in the country. The PHASER team has found that each VA is unique and diverse, but, through this program, the testing will be aimed to be scalable to different settings – rural, urban, academic affiliated, and nonacademic affiliated VA clinics and hospitals. Regardless, those Veterans that have been tested will have the results in their chart for their benefit beyond the conclusion of the program.
Providers and pharmacists play a particularly crucial role in applying the PGx results so that their patients can receive the healthcare benefits of this application of precision medicine.
“We have developed a large portfolio of educational materials and a toolkit within the electronic health record so that frontline providers know how to access PGx test results, how to use them in clinical care, and where to go for help when they need it,” said Dr. Voora.
Veterans receiving care at a VA should contact their local VA health care provider if they are interested in learning more about the PHASER program.
A study about the PHASER program was recently published in the Future of Medicine Pharmacogenomics Journal. Read more about it here.
If you have questions about the PHASER program, please reach out to Deepak Voora (Deepak.voora@duke.edu)