R38 scholar Aaditya Khatri, MD, PhD, is the lead author on a new study that offers a potentially novel therapeutic strategy for the prevention or treatment of chronic lung allograft dysfunction (CLAD), the leading cause of death in lung transplant recipients.
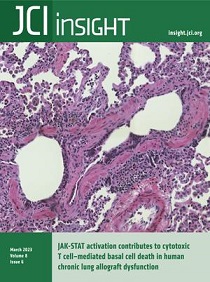
The March 22 cover of JCI Insight is devoted to the study: JAK-STAT (Janus kinase-signal tranducer and activator of transcription) activation contributes to cytotoxic T cell–mediated basal cell death in human chronic lung allograft dysfunction.
While lung transplantation extends survival and improves the quality of life in patients with advanced lung disease, long term survival after transplantation is limited by the onset of CLAD, a manifestation of chronic rejection in the lung for which there are no targeted treatments to prevent or treat the disease.
In this study, the genome was sequenced from individual lung cells from patients with CLAD undergoing a second or third transplant, allowing researchers to identify novel pathways and cell-cell interactions driving progression of disease.
They found that the JAK-STAT pathway is switched on in lung airway stem cells and leads to immune cell targeting and cell death of these important stem cells. In the absence of these stem cells, the lung is not able to repair or regenerate normally, leading researchers to believe that this mechanism plays an important role in the progression CLAD. Targeting this pathway with inhibitors may lead to new therapies for patients to prevent and treat CLAD, they conclude.
The Power of Doing Science at Duke Medical School
“This project illustrates the power of doing science in the Duke School of Medicine,” says Khatri, a 2018 graduate and now fourth-year internal medicine resident who completed training in the Duke Medical Scientist Training Program (MTSP). “Science is a team sport and Duke has one of the most collaborative environments of any institutions in the country.” Khatri begins his tenure as a pulmonary fellow in July.
Duke investigators teaming with Khatri on the study include Jamie L. Todd, Fran L. Kelly, Andrew Nagler, Zhicheng Ji, Vaibhav Jain, Simon G. Gregory, Kent J. Weinhold, and Scott M. Palmer, from the Department of Medicine, the division of Pulmonary, Allergy and Critical Care Medicine, Duke University Medical Center, Duke Clinical Research Institute, the Department of Biostatistics and Bioinformatics, Duke Molecular Physiology Institute, and the departments of Neurology and Surgery.
Dr. Palmer adds research like this is possible because of the outstanding Duke clinical lung transplant program that includes world-class cardiothoracic surgeons, transplant pulmonologists and a large multi-disciplinary team of faculty and staff across the health system. In addition, Duke’s exceptional scientific resources supported the work including the BioRepository and Precision Pathology Center for expedited access to valuable lung specimens immediately after surgery, the research coordinators for consenting patients and processing patient specimens, the Molecular Genomics Core led by Simon Gregory to perform the sequencing experiments, and the Biostatistics and Bioinformatics Department for data analysis.
The R38 Research Pathway
The publication is particularly notable because Dr. Khatri completed the research as an internal medicine resident on the R38. The R38 program was established as a solution to retain and develop physician scientists across the multiple departments originally led by Drs. Harpole, Palmer, and Permar.
Funded by the NHLBI and NIAID, the Duke team was fortunate to receive two of the first R38 awards given to any institution in 2018 and began offering the Duke R38 Research Pathway for residents committed to a career as a physician investigator, with additional oversight for trainees within the DOM led by Maria Rapoza, PhD.
Dr. Rapoza notes these awards provide a dedicated funding mechanism and 80 percent protected research time over two years of residency training. This allows R38 researchers to get a three to four-year head start on their research compared to colleagues who have to wait until the completion of clinical training in fellowship. She also said that all of the appointees who have graduated from R38 training have remained at Duke for subspecialty fellowship, with a commitment to pursue academic research.
“We’re nurturing the next generation of physician scientists,” Rapoza said. “It's a very hard path to follow to become a physician scientist. That's why more people don't do it. There have been a lot of resources that have coalesced around our appointees, not just funding. We have such a supportive community of more mature physician scientists like Scott himself. The Department of Medicine has such a strong track record of supporting physician scientists. That's not something a lot of institutions are able to do.”
Dr. Palmer notes the NHLBI R38 has already been successfully renewed for a second cycle based on the success of the program and its trainees over the past five years, and the NIAID award is under review for renewal. In addition, Duke has received two additional institutional R38 awards ensuring this pathway will continue to grow to support the success of the next generation Duke and DOM physician investigators.
Feature photo: Study authors, from left to right, are Andrew Nagler, Aaditya Khatri, Scott Palmer, and Jamie Todd.