About the Center

The primary focus of the Radiation Countermeasures Center of Research Excellence (RadCCORE) program is to support basic, translational and applied research leading to new medical countermeasures against radiological and nuclear exposures due to terrorist attacks.
The underlying driving force is to bring “deliverables” to the national stockpile to mitigate the effects of radiation induced injury. We have structured this research consortium as a multidisciplinary research center to move candidate products through the regulatory process, conduct basic and translational research to identify new counter measures to evaluate countermeasures and underlying biology, and provide new or expanded education resources to improve expertise in radiobiology.
In order to achieve this goal, leading scientist in the area of radiation biology, health physics, stem cell biology transplantation and immunology, have united to form one of the most, if not the most, comprehensive inclusive, inter-institutional and interdisciplinary Center for Medical Countermeasures Against Radiation (CMCR). We have formed the RadCCORE consortium to collectively and collaboratively increase possible agents to detect, mitigate and treat those people exposed to deterministic doses of radiation. RadCCORE is a network of academic medical centers (Duke University, University of North Carolina, and Wake Forest University). This core group will be supported by affiliate members and consultants from other academic institutions, national research laboratories, and private enterprises.
Research Projects
Nelson Chao, MD, MBA
Duke University
Principal Investigator
In the event of a nuclear accident or a radiological attack, the exposure to ionizing radiation can cause acute damage to radiosensitive tissues that have rapid turnover rates, including the hematopoietic (H) system and gastrointestinal (GI) tract. After irradiation, an insufficient regeneration of either the hematopoietic system and/or the GI tract can lead to death within a few weeks, which is termed the acute radiation syndrome (ARS). Although significant progress has been made to understand mechanisms underlying the ARS, no FDA approved therapy is available to treat both the H-ARS and the GI-ARS when given at least 24 hours after irradiation.
At this time point, the majority of tissue stem/progenitor cells will already be dead. Therefore, there is an urgent need to develop novel medical countermeasures (MCMs) that target master regulators of tissue regeneration in response to radiation injury. The long-term goal of this project is to develop a novel class of MCMs that mitigate both the H-ARS and GI-ARS by targeting calcium/calmodulin-dependent protein kinase kinase 2 (CaMKK2). We have shown that inhibition of CaMKK2 by genetic deletion or by the small molecule inhibitor STO-609 is sufficient to stimulate hematopoietic regeneration and mitigate the H-ARS. Remarkably, our preliminary data indicate that deletion of Camkk2 specifically in myeloid cells is sufficient to facilitate blood cell formation following total body irradiation. More recently, we found that deletion of Camkk2 also protected mice from the GI-ARS. Of note, outside the brain, the expression of CaMKK2 is restricted to a small number of cell types, including macrophages and epithelial tuft cells, which share the ability of tuning the regeneration rate of hematopoietic and intestinal stem cells. Based on these findings, we hypothesize that CaMKK2 is an important druggable target to regulate the behavior of hematopoietic and intestinal stem cell niches, and blocking this enzyme 24 hours after irradiation will be sufficient to facilitate tissue regeneration in response to radiation injury. We will test this hypothesis using sophisticated mouse models, CaMKK2 inhibitor, along with primary bone marrow cells and intestinal organoids from human donors. Using these combined approaches, we will define mechanism(s) by which CaMKK2 expressed in myeloid cells mitigate H-ARS, and will determine the impact of acute Camkk2 loss in tuft cells after irradiation on the development of GI-ARS. By completing this grant, we expect to gain new insight into the role of CaMKK2 in regulating both the H-ARS and GI-ARS. More importantly, by more comprehensively understanding mechanism(s) underlying the effects of CaMKK2 inhibition on mitigating the ARS, we will lay the foundation for approval of STO-609 as a medical countermeasure against radiation under the FDA’s Animal Rule.
Benny Chen, MD
Duke University
Principal Investigator
The misuse of ionizing radiation or nuclear devices as weapons of terrorism has been recognized as a major U.S. public health threat. The greatest risk to these victims of radiation exposure is the hematopoietic acute radiation syndrome (H-ARS), which results in life-threatening complications such as infections and refractory bleeding. Specific therapies directed at H-ARS to accelerate hematopoietic regeneration following radiation injury have been few. Since marrow endothelial cells can govern hematologic recovery after irradiation without homing to the bone marrow, endothelial cells can mediate their radioprotective effects through elaboration of hematopoietic cytokines or soluble factors. Another mechanism of cellular communication is through transfer of proteins and nucleic materials via secretion of extracellular vesicles (EVs). EVs range in size from 100-250 nm and bear both nucleic acids and proteins that have potential to regulate neighboring cells. We hypothesize that ECs exert their regenerative effects through EVs. We have shown that treatment of irradiated hematopoietic stem/progenitor cells with either syngeneic or allogeneic EVs from genetically distinct mice results in comparable expansion of the stem cell pool, suggesting they could be immunologically tolerant. Compared to control mice treated with granulocyte colony stimulating factor (G-CSF), it is possible that EVs are at least comparable and are likely superior to G-CSF for prolonging survival after lethal-dose irradiation. Our overriding goal is to demonstrate the radiotherapeutic capacity of EVs. In doing so, we will develop a cellular-based therapy for H-ARS with potential for off-the-shelf delivery to victims in the setting of a mass casualty disaster.
Jenny Ting, PhD
University of North Carolina - Chapel Hill
Principal Investigator
Multi-organ radiation-induced injury is a major threat during targeted terror attack, and adaptive and innate immunity are increasingly found to play a key role in this process. Innate immune receptors collectively referred to as Pathogen Recognition Receptors (PRR) have undergone an explosive discovery phase. Prominent PRR families include the membrane bound Toll-like receptors (TLR) which interact with extracellular ligands. These have been extensively studied in infection and inflammatory diseases, and their impact on radiation-induced damage has emerged in the last few years. Post-exposure, radiation not only causes acute injury but also delayed injury such as fibrosis and defective cellular and immune development. We and others have explored the roles of TLRs in radiation and unexpectedly found that certain TLRs and their ligands are protective of radiation-induced damage involving both the hematopoietic system as well as the gastrointestinal tissues. In addition to TLR ligands, we have also isolated beneficial microbiota and metabolites from animals that survived lethal radiation, and propose to explore if these microbes and their metabolites can mitigate radiation damage. This proposal will focus on the use and mechanism of TLR ligands, commensal microbes and their metabolites as radiation mitigators that can reduce radiation induced damage.
David Kirsch, MD, PhD
University Health Network, Toronto
Principal Investigator
In the event of a radiation disaster or attack, high dose radiation exposure to humans causes Acute Radiation Syndrome (ARS). The hematopoietic system and gastrointestinal (GI) tract are among the most vulnerable tissues to radiation injury due to the presence of cycling stem cells that are sensitive to radiation. Loss of regenerative capacity in these organs leads to lethal toxicity. For example, damage to the bone marrow from total body irradiation leads to the hematopoietic syndrome. High doses of radiation to the abdomen results in GI syndrome characterized by damage to the intestinal epithelium, loss of mucosal barrier, and sepsis. While, medical countermeasures to mitigate the hematopoietic syndrome are available, there are currently no FDA approved therapies to mitigate the GI syndrome.
We have demonstrated that p53 mediated expression of the cell cycle inhibitor p21 in GI epithelial cells is critical for survival of the GI syndrome. High p21 expression prevents damaged cells from progressing through mitosis and succumbing to mitotic catastrophe. In contrast, radiation kills p21-low, fast cycling LGR5+ GI stem cells in the base of the crypts. When these cells are lost, regeneration of the intestinal epithelium is dependent on a slow-cycling, and thus radioresistant, cell population that resides higher in the crypt. Therefore, identifying the GI epithelial cell type that is preserved by high p21 expression and capable of supporting tissue regeneration following injury will be important for developing mitigation strategies for GI syndrome.
Recently published single cell RNA sequencing data from irradiated small intestine epithelial cells in mice identified Clu+ revival stem cells as slow cycling cells with high p21 levels that survive 24 hours and proliferate after high dose irradiation. Clu+ cells are capable of regenerating LGR5+ stem cells after injury and loss of this cell type sensitizes mice to GI syndrome lethality. Clu+ cells rely on the Yap1/Hippo signaling axis for maintenance and therefore we hypothesize that modulation of this pathway will mitigate the GI syndrome. In addition, Dclk1+ tuft cells were also identified to have high p21 expression and survive high dose radiation.
These cells are chemosensory and secretory cells that support renewal of the GI epithelium following irradiation by maintaining the stem cell niche. We hypothesize that p53 regulation of p21 in these cell types is critical to intestinal recovery following radiation injury and that targeting these cells for mitigation is a promising strategy. We propose to dissect the mechanisms by which Clu+ revival stem cells and Dclk1+ tuft cells function to promote renewal of the GI epithelium after radiation injury using sophisticated genetically engineered mouse models. We will use targeted approaches with small molecule drugs in vivo and CRISPR/Cas9 screening organoid cultures to identify novel mitigator targets that function specifically in these cell types to reduce lethal GI toxicity.
Core Services
A long-term goal for RadCCORE is to establish the leaders, the projects and the infrastructure to have a vibrant, responsive, and effective research and development organization as a member of the CMCR national center group that in future years can respond to these threats. To this end we have established a number of Cores to support the research projects of RadCCORE.
Nelson Chao, MD, MBA
Core Director
The Radiation Countermeasures Center of Research Excellence (RadCCORE) is an interdisciplinary, multi-institutional organization made up of Duke University, University of North Carolina- Chapel Hill, and Wake Forest University. Thus RadCCORE is a complex organization that requires a well-organized, and efficient Administrative Core (Core A) to ensure its success. The overall goal for Core A is to create and implement administrative and leadership mechanisms that will foster effective interactions among the RadCCORE investigators and institutions to ensure a productive research effort. To accomplish this, Core A will be responsible for the overall organization, management, decision-making, communications, and periodic evaluations within RadCCORE. Core A will be responsible for oversight of data sharing, protection of intellectual property, and involvement of institutional resources. Core A will also organize and support the activities of the External Scientific Advisory Group. Dr. Nelson Chao, the Principal Investigator of this application, will serve as the Core Leader of the Administrative Core.
Joel Ross, PhD
Program Director
Phone: 919-668-1722
Brittany N Jackson
Grants Manager
Phone: (919) 684-5066
Jennifer Kajcienski
Administrative Assistant
Phone: 919-668-1040
Zhiguo Li
Core Director
The overall goal of the Biostatistics Core (Core B) is to promote scientific rigor in the conduct of RadCCORE research and to ensure the integrity of results. To this end, Core B will offer state-of-the-art biostatistics and bioinformatics support to RadCCORE projects and cores. This includes assistance in the statistical design, analysis and interpretation of data obtained from clinical, pre-clinical and laboratory studies, as well as molecular data obtained from genomic experiments and cell assays. Core B will also provide ongoing consulting and educational services to all RadCCORE investigators. Core B will use existing computing infrastructure resources as an efficient means to support RadCCORE research. It will also strive to take advantage of the vast amount of technical expertise in biostatistics, bioinformatics and information sciences within Duke University.
Andrew Macintyre, Ph.D.
Core Director
The Immune Monitoring Core for RadCCORE is comprised of technologies and services offered by two service laboratories within the Duke Human Vaccine Institute (DHVI): the Flow Cytometry Facility and the Immune Reconstitution and Biomarker Facility. In this competitive renewal (y6-10) we have focused the scope of Core offerings based on project utilization and future needs. The Immune Monitoring Core (Core C) will centrally provide RadCCORE investigators with high quality, state-of-the-art cell sorting, multiplex cytokine/chemokine assays, and T cell receptor gene expression analysis for their basic and applied research efforts. In addition to providing these services, the Core will be instrumental in developing new methodologies and making them available to RadCCORE Investigators. Administrative oversight for the Core will institute a charge-back mechanism for services provided in excess of budget to remain revenue neutral and financially compliant. In addition, the Core will utilize our innovative FacMan-Facility Manager web application created by the Duke Human Vaccine Institute to schedule/request core work, maintain accurate and compliant records of uses and projects, and invoice for services rendered.
Aims of the Immune Monitoring Core are to:
- Provide state-of-the-art, multi-color, fluorescence activated cell sorting support for basic or translational research conducted by Duke RadCCORE investigators. This includes high-speed sorting on our 8-color BD FACSVantage SE and 13-color BD FACSAria. Protocols are available for surface and intracellular marker analysis of mouse, rat, human and non-human primate cells.
- Provide targeted multiplex protein array profiling of biological samples, such as tissue culture supernatant, serum/plasma, and lung lavage fluid, using our BioPlex bead array reader (BioRad). This instrumentation and Luminex bead technology has the capability of simultaneously quantifying up to 100 distinct analytes (e.g. cytokines, chemokines, hormones, signaling transduction proteins) in a single 50ul sample. Reagents and protocol are maintained in the Core for analysis of mouse, rat, pig, human and non-human primate samples.
- Provide T cell immune reconstitution monitoring in mice, humans and non-human primates. Specific assays include T cell receptor excision circle quantification on our real-time Optical I-Cycler (BioRad), and repertoire analysis of peripheral T cell receptor beta variable gene utilization.
By working in collaboration with the RadCCORE scientific program user base we will develop and optimize their specific assays and more effectively utilize the state-of-the-art instrumentation offered by the Immune Monitoring Core. Critical to all three aims is a commitment to training and ongoing development of new assays to anticipate and meet the future needs of the RadCCORE investigators.
For a detailed description of the facilities visit:
Mark Cline, DVM, PhD
Core Director
The Primate Studies Core facilitates the conduct of late-stage preclinical studies of mitigators of radiation damage in nonhuman primates, following the specific priorities of the RadCCORE consortium and other CMCRs nationwide, including since 2007 long-term care and study of animals surviving high-dose irradiation at other institutions. Because of the high degree of genetic and physiologic similarity of nonhuman primates to human beings, this resource is a critical component of translational assessment of candidate deliverable agents, in an experimental setting under which relevant doses of whole-body irradiation can be given to healthy subjects. Core investigators have unique skills in the experimental use and clinical medicine of nonhuman primates, including irradiation, veterinary medical care and management of myelosuppressed animals, comparative pathology of primates, pathology of radiation injury, biochemistry, clinical pathology and endocrinology of primates, and adaptation of molecular biologic techniques to the primate model. Core services include acquisition and maintenance of specific-pathogen-free nonhuman primates, exposure of animals to radiation, administration of therapeutic interventions, and clinical and pathologic assessments of treatment outcomes, including necropsy/tissue collection and sharing for baseline characterization of radiation responses and assessment of mitigating interventions.
The Core also provides extensive data management services for primate studies, including data and tissue sharing. Please complete this form to request samples:
Education & Training
RadCCORE sponsors periodic training events, seminars, and workshops.
The Nuclear Threat Initiative is working to reduce the global threats from nuclear, biological and chemical weapons and is co-chaired by Ted Turner and Sam Nunn. Use this site to get the facts, get informed and get involved.
Radiation Emergency Assistance Center/Training Site (REAC/TS)
REAC/TS trains, consults, or assists in the response to all types of radiation accidents or incidents. The Center's specially trained team of physicians, nurses, health physicists, radiobiologists, and emergency coordinators is prepared around-the-clock to provide assistance on either the local, national, or international level.
Emergency Response
This section provides information for the general public and for health care professionals. Please look at our Education and Training resources too.
The threat of terrorism is now a real and constant danger that we must face together. Perhaps the most frightening situation to imagine is the use of radioactive materials by terrorists. The best defense against this possibility starts with knowing the facts and being prepared. A great place to get started is with this "Introduction to Radiological Terrorism."
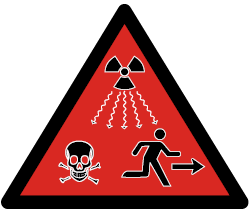
The ISO (International Standard Organization) has just standardized a new symbol aimed at warning everyone - particularly non-specialists - of the danger posed by a source of radiation. It is a triangle on a red background containing the symbol for radioactivity (the 'clover') with an indication of radioactive emissions, a skull and crossbones and a man running away. This symbol may be used in addition to the 'radioactive clover'.
Protecting Yourself and Your Family
If a radiation emergency occurs, people can take actions to protect themselves, their loved ones, and their pets. Emergency workers and local officials are trained to respond to disaster situations and will provide specific actions to help keep people safe.
From the Centers for Disease Control and Prevention (CDC.gov)

The Radiation Injury Treatment NetworkSM (RITN) provides comprehensive evaluation and treatment for victims of radiation exposure or other marrow toxic injuries. RITN develops treatment guidelines, educates health care professionals, works to expand the network, and coordinates situation response. RITN is a cooperative effort of the National Marrow Donor Program® (NMDP) and The American Society for Blood and Marrow Transplantation (ASBMT).
From the Centers for Disease Control and Prevention (CDC.gov)
Radiological Terrorism: Just-in-Time Training for Hospital Clinicians provides guidance on responding to a radiological incident. This presentation includes a brief overview of the principles of radiation, medical response scenarios, and information on patient triage and treatment.
