
1-Year Clinical Fellowship Program
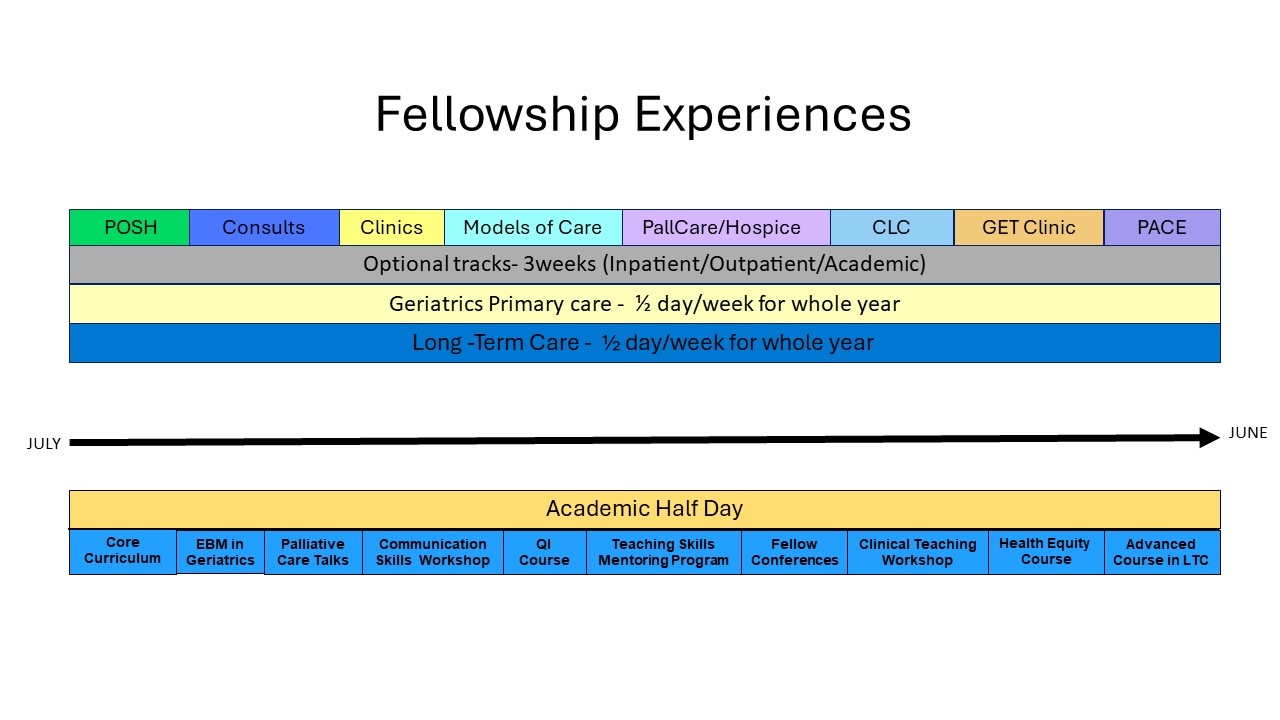
This one-year fellowship provides trainees with in-depth experiences with the full spectrum of patients and problems that geriatricians are likely to encounter, across a variety of clinical settings. Upon successful completion of the year, fellows are prepared for careers caring for older adults in and across a variety of settings and eligible to take the American Board of Internal Medicine Geriatric Medicine Certification Exam.
Why I Chose Duke
"My Duke Geriatric fellowship has been one of my best decisions that I have made in my life. The rotations are set up well to include various care models and settings. You get to work alongside with master clinicians that are full of passion in their work. All the faculties attendings that I came across had great minds, yet humble and down to earth, approachable, and offered fantastic mentorship. There are many opportunities to spend personal time together with the faculty and truly made me feel like a part of a big family. The fellowship program not only prepared me well for the career as a geriatrician, but also helped me find my true passion. It was a life changing time for me, and I would recommend Duke geriatric fellowship to anyone without any reservation."
Sungyub "Charles" Lew, MD--Fellowship Alumni