
Group visits have been around more than a decade, particularly for management of chronic illnesses such as diabetes. Gaining in popularity, some say the greeting at the next appointment will be “the doctor will see all of you now.”
These researchers, led by Dr. Will Yancy, are taking a new approach with a serious focus on weight management as the primary goal. The team has recruited more than half of the participants and expects to complete the outcome assessments next summer. Here is the project outline.

Project Name: Jump Starting Shared Medical Appointments for Diabetes with Weight Management
Project Acronym or Short Title: JUMP START
Funding Agency: VA Health Services Research
PI(s): Will Yancy, MD
Project Staff: David Edelman, MD Co-Investigator), Matthew Crowley, MD (Co-Investigator), Matthew Maciejewski, PhD (Co-Investigator), Corrine Voils, PhD (Co-Investigator), Cynthia Coffman, PhD (Co-Investigator), Marsha Turner and Jennifer Zervakis (Project Coordinators), Leslie Gaillard (Clinical Dietician), Jamiyla Bolton (Coordinator), Elizabeth Strawbridge (Dietician/Research assistant), Teresa Hinton (Research RN), Amy Jeffreys (Statistician), Jennifer Lindquist (Statistician), Aviel Alkon (Programmer), Lesa Powell (Programmer), and Anna Beth Barton, MD (Fellow).
Brief Description: Shared medical appointments (SMAs) are a type of group medical visit that show promise for providing efficient, high-quality health care. SMAs involve groups of patients who share a common chronic condition and meet over time to receive education, self-management skills, and medication management to improve clinical outcomes. SMAs for patients with diabetes improve glycemic control and blood pressure. Although these SMA programs sometimes included diet and physical activity counseling, weight management was not a primary goal, and weight typically was not reduced. Weight management is very important in patients with type 2 diabetes because it is a predictor of improved blood sugar control and has been associated with lower risk for complications of diabetes, independent of blood sugar control. The Jump Start research program will examine whether an intensive, group-based weight management program using a low carbohydrate diet followed by an SMA intervention (WM/SMA arm) is comparably effective to the SMA intervention alone for improving glycemic control, while reducing antiglycemic medication, decreasing hypoglycemic events, and lowering healthcare costs. 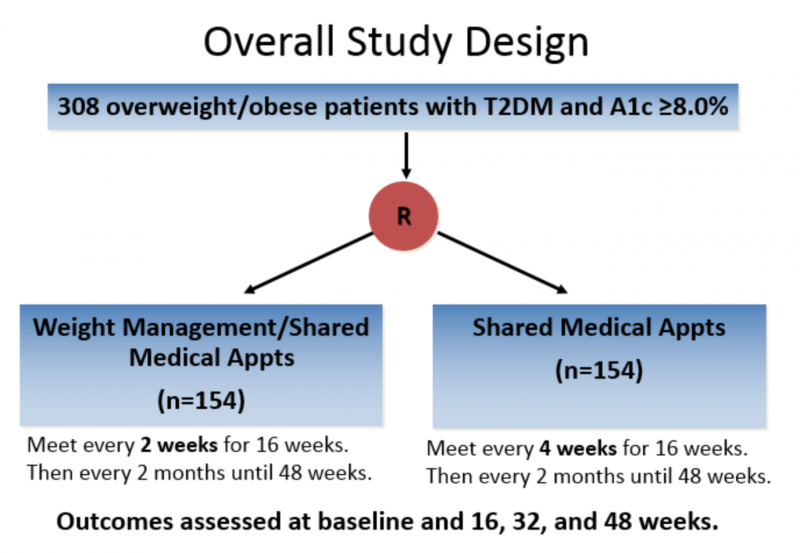
Intervention: 308 overweight VA outpatients with uncontrolled type 2 diabetes (Hgb A1c >8.0%) will participate in this RCT. The SMA group visits will occur every 4 weeks for 16 weeks and then every 8 weeks for 32 weeks for a total of 9 visits. Sessions will be led by a physician and trained interventionists, and will include educational topics related to diabetes management, self-management training, and medication adjustment. The WM/SMA group will meet every 2 weeks for 16 weeks focusing on a low carbohydrate dietary pattern, and then every 8 weeks for 32 weeks for a total of 13 visits. After 16 weeks content will shift to the SMA intervention content but weight management will continue to be addressed.
Outcomes: The primary outcome is glycemic control assessed by hemoglobin A1c assessed at baseline and at 16, 32, and 48 weeks. Secondary outcomes include hypoglycemic events, changes in total anti-glycemic medication burden, weight and healthcare costs.
We have recruited 185 Veterans from the Durham VAMC as of June 2016. Final outcome assessments will be completed August, 2017. Questions about this study can be directed to the Study Coordinator at (919) 286-0411 ext 6174.
_____________________________
Tell us about your clinical research or your projects in education or clinical practice.
Write to GIM Communications Strategist, Clare Il’Giovine