
Post submitted by Patrick Hemming, MD, Duke GIM Assistant Professor of Medicine.
This month’s meeting of the Society of General Internal Medicine provided a showcase for excellent work by Duke students, residents and faculty, which was highlighted here. I presented the Duke Outpatient Clinic (DOC) as a hub for primary care innovation. In a poster, we demonstrated our process of integrating new behavioral health services into the clinic.
How we did this
Our integration pilot brought 2 new masters-level behavioral health consultants (BHCs), Ashley Cyr and Joy Long-Vidal into our clinic to assist with counseling and supporting our patients with a wide variety of behavioral health conditions. Their scope of practice ranged from common mental health concerns (depression and anxiety) to helping care coordination for patients with severe persistent mental illness (schizophrenia and bipolar disorder), as well as assisting with alcohol and substance use disorders and tobacco cessation. Frequently, these services involved meeting with multiple members of a patient’s family to assist with complex interpersonal challenges.
 In March 2016, Ashley and Joy joined the practice and expanded the DOC’s capacity to improve patient-centered care. Physician champion Larry Greenblatt initiated a partnership with Alliance Behavioral Health, Durham County’s Medicaid Local Management Entity. Insurers like NC Medicaid are increasingly trying to bridge the historical and false division of “physical” and “mental” health by funding and encouraging behavioral health integration. Integration allowed the DOC to begin routine screening for behavioral health conditions using a one-page patient form with questions about depression, anxiety, alcohol and substance uses, and questions about memory concerns and social determinants of health (lack of access to housing, food, medications).
In March 2016, Ashley and Joy joined the practice and expanded the DOC’s capacity to improve patient-centered care. Physician champion Larry Greenblatt initiated a partnership with Alliance Behavioral Health, Durham County’s Medicaid Local Management Entity. Insurers like NC Medicaid are increasingly trying to bridge the historical and false division of “physical” and “mental” health by funding and encouraging behavioral health integration. Integration allowed the DOC to begin routine screening for behavioral health conditions using a one-page patient form with questions about depression, anxiety, alcohol and substance uses, and questions about memory concerns and social determinants of health (lack of access to housing, food, medications).
 Our results
Our results
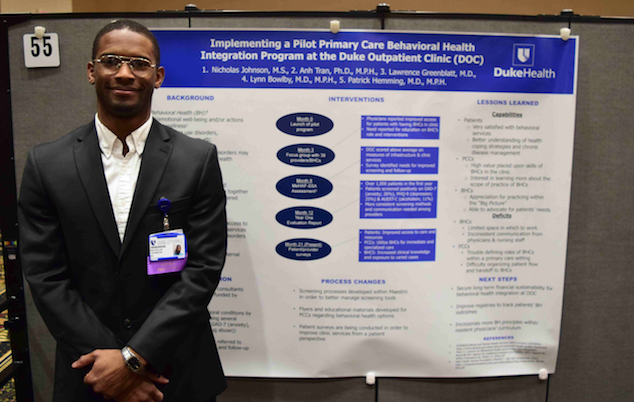
In the first year of the pilot, over 3000 patients completed screenings, demonstrating that more than 25 % of our patients had a mental health or substance abuse concern. Our residents and attending physicians began referring patients who had positive screens to the BHCs, who could spend extra time to evaluate and counsel patients. Frequently, their initial assessment would result in at least one follow-up visit to evaluate progress with treatment and to provide further counseling. In year one, Ashley and Joy worked with over 1000 patients. Patient surveys were glowing with satisfaction and gratitude. Over half of patients reported that they would not have otherwise accessed behavioral health services. Nick Johnson (pictured) designed and collected our patient surveys as part of his Master’s Degree in Health Sciences. He will be beginning medical school Duke in 2018. He also presented our work at the Duke Patient Quality and Safety Conference in March 2018.
Importance for Trainees
Behavioral health integration also provided unique learning experiences for the 70+ residents who practice at the DOC. In focus groups and surveys, the residents were pleased to see their patients getting better support. Residents reported eagerness to improve their understanding of the BHCs range of practice. These requests prompted us to move the BHCs’ desks into the precepting room, where they would be available for consultation as residents discussed patient cases with their attendings, a new learning laboratory for the DOC.
Next steps
Due to some changes in the funding for North Carolina Medicaid, the DOC’s behavioral health integration pilot ended temporarily in March 2018. Next steps for behavioral health integration at Duke will likely need to leverage several important national developments, including Medicare’s deployment in 2018 of new billing codes for behavioral health care management services.
Read more about new developments
Check out the next blog post where I describe the Special Symposium that I led at the 2018 SGIM annual meeting here. The subject is new developments in primary care behavioral health integration that can provide financial sustainability for practices and health systems.