From the Director

Hey Everyone!
We are at the end of Fun-bruary! The days are getting longer, it is a bit brighter in the morning and in the evening … and only a few short weeks until Match Day! Thanks all for helping out with keeping it a bit lighter in February, traditionally the gloomiest month of the residency year. Check out AJ on Dress Like your Attending Day, as well as fun pics from Gen Med. Amy Lee, Jeja Syeda and Manisha Bhattacharya had some haiku performance art this weekend (unfortunately no photo evidence) as well.

We have two new members of the Duke family! Shown here are proud papas Jacob Kauffman and Mike Powers. Although you can’t tell, they are holding the wrong babies! Welcome Michael Francis Powers and Elizabeth Laura Kaufman - "Elle"!

Kudos this week from Amy Lee to her Gen Med interns Jeja Syeda (who also did a great intern report!), Zach Il’Giovine, and Manisha Bhattacharya, and from Div Patel to his VA GM intern Phil Liu and to colleague Lauren Ring for great work.
Major Duke congratulations to our ACP crew! What a fantastic showing by Duke (see the photos), with Eric Black-Maier winning the research competition and Nick Turner winning best overall! Also, Jenn Rymer represented with second place in the poster competition! Our super smart trivia bowl crew (EBM, Nick Turner and Peter Hu) came in second place in the competition by a mere difference of 10 points! Great job to all.

Had a fun JAR dinner at Bar Virgile with Ani Kumar and the ladies (Linda Koshy, Kahli Zietlow, Stephanie Li and Lauren Ring. Then we got to have a fun SAR get together on Sat night at my house, finally getting to cash in on last year’s charity auction! Thanks to Andrea Sitlinger for getting everyone together.
The Duke Carolina game is at 6:30 on Saturday! Join us at Motorco as we cheer on Duke (you are welcome to join us if you are one of the #dukefamily who happens to cheer for the perenially underachieving down the street neighbor too)
This week’s pubmed from the program goes to the all who represented us so well at the ACP! Elieth Martinez, Nick Turner, Ali Saadi, Taylor Bazemore, Maggie Moses, Eric Black Maier, Rajiv Agarwal, Amy Jones, Emily Kinsey, Eric Fountain, Adva Eisenberg, Rachel Hu, Peter Hu, Sarah Nouri, Amanda Boyd, Ankeet Bhatt, Katrina Abril, Jason Zhu, Liz Kotzen, Tracey Liljestrom, Joanne Wyrembak, and Kahli Zietlow as well as med students Moeiz Ali,Benjamin Andrew, Matthew Detter, Katie Falloon and Kun Wei Song.
Have a great week!
Aimee
What Did I Read This Week?
Submitted by Christopher Hostler, MD
“I don’t take the flu shot because every time I do, I get the flu.” “I don’t need the flu shot, I’ve never gotten the flu before.” “I got the flu shot last year and still got the flu, so I’m not taking it anymore.”
How many times have you heard any/all of the above statements from your patients? And how many times have you concussed yourself as you bang your head against the wall trying to convince your patients to help you help them?
This week in CID, a large multi-center prospective study on the effectiveness of US influenza vaccine from the 2012-2013 season was published (Petrie et al. Illness severity and work productivity loss among working adults with medically attended acute respiratory illnesses: US influenza vaccine effectiveness network 2012-2013. Clin Infect Dis (2016) 62 (4): 448-455.). This study included 1548 employed adult patients who presented to ambulatory care centers with an acute respiratory illness of <=7 days duration. Patients had throat and nasal swabs done for viral identification, were treated for influenza if clinically indicated, and were surveyed 7 days after enrollment on their health and activity status, sleep quality, as well as how much time out of work they required during the illness (work productivity loss).
Not surprisingly, those who had influenza had worse health and activity statuses and more missed work hours than those with non-influenza illnesses. Also not surprisingly, fewer patients who had been vaccinated against the flu tested positive for influenza than those who were not vaccinated. What may be useful in convincing your patients to get the flu shot was the fact that patients who had influenza and had been vaccinated had a lower severity of illness than those who were not vaccinated (as evidenced by a statistically significantly better “health score” at 7 days after enrollment, though no change in work productivity loss).
Why, you may ask, am I bringing this up at the end of February? As evidenced by the NC Influenza Surveillance Network, we appear to just now be heading into peak flu season, which is later than it has been in previous years.
So when your patient tells you “oh I don’t want the flu vaccine because last year I got the flu even though I got the shot” or “I’ve never had the flu, so I don’t need the shot,” remind them that they’re missing the whole point of the vaccine. It's not to prevent all cases of flu (though that would be great), it's to reduce the mortality and morbidity of the flu. We know that the 2009 California H1N1 and the 2012 Texas H3N2 strains are more virulent and cause more fatalities than some of the other H1N1 and H3N2 strains, so we vaccinate against those. This paper is evidence that not only does the flu shot reduce the likelihood that you’ll contract the flu, but it also reduces the severity of illness should you contract the flu.
The bottom line is that with mortality rates that still exceed 50,000/year, there are multiple reasons to get a flu shot and very few not to get one. And if my 2 year old can take it like champ, so can your 40 year-old patient.
QI CORNER
Thank you SO much to those of you who have already filled out the paging survey! We really appreciate your input and we are already learning from the pilot on 4300.
I will be meeting with the ACLT group soon to start brainstorming on next years "sharepoint" outpatient QI project. If you have ideas or want to join the discussion, please email me so we can include you in the meeting.
CLINIC CORNER

by Daniella Zipkin, MD
Hi everyone! Hope things are going well. As always, please forward feedback or comments about ambulatory rotations over to me. No issue is too small, sometimes the little details really matter!
Gen Med Careers Night!!
Mark your calendars for March 15th, 6:30-8:30 pm, Med Res Library! Sharon Rubin is organizing a career planning social event, dinner will be served. If you are considering hospital medicine, primary care, or academic general internal medicine (including health services research, quality improvement, education or administration) please join us for food and drink and networking.
SGIM Annual Meeting
The Society of General Internal Medicine is the academic home for GIM. It’s the primary forum for generalists to share their work in research, education, or clinical practice innovations. This year the meeting is May 11-14 in Florida. Matt Atkins will present a poster entitled “Adherence to USPSTF and ACIP Clinical Guidelines in Resident Clinics”, and Alex Cho will lead the DOC redesign team with his oral presentation entitled “A Needs-Based Resident Clinic Redesign Results in Improved Patient Utilization of Care and Increased Resident Satisfaction”. Congratulations!!
Duke alphabet soup – PDC? DPC? What’s it all about?
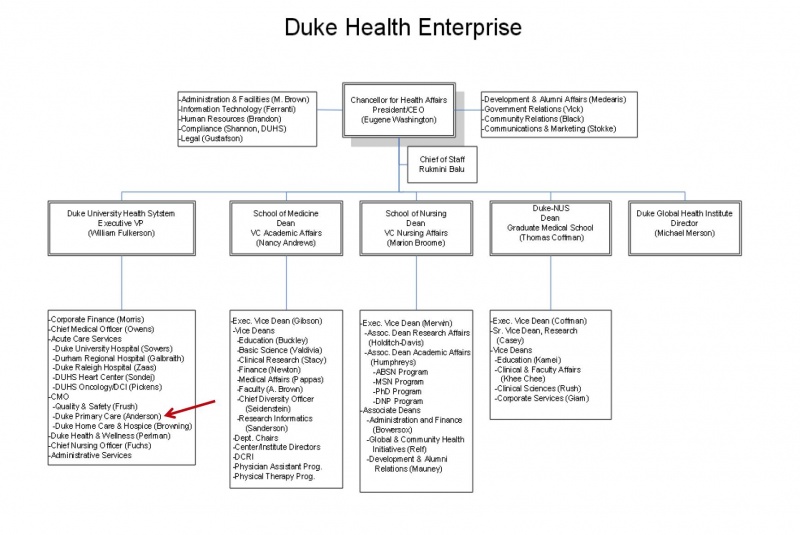
Armando and Jen and I recently met with folks from Duke Primary Care to review ways in which we can collaborate more and offer you all more experiences in outpatient QI, clinical primary care, and practice management. At one point Armando pointed out that many of our residents may not know what the PDC vs. DPC are. I admit, sometimes I’m confused too. So we are putting together a little road map to try to clarify. In the words of Kevin Shah:
“Duke Primary Care (Including Pickett Road, but NOT DOC), Duke Hospitalists and Duke Palliative Care are all employees of DUHS. Physicians at the DOC, Duke Family Medicine, and faculty in every other specialty department belong to the Private Diagnostic Clinic. You will notice the PDC is not on this Org chart because they are a separate organization from DUHS. Faculty who have a significant research / teaching role may draw some of their salary from the School of Medicine.”
Here is the organizational chart:
From the Chief Residents
Grand Rounds
Friday, March 4 - CMR, Chief Residents
Noon Conference
| Date | Topic | Lecturer | Time | Vendor |
| 2/29/16 |
MKSAP |
Chiefs |
12:00 | Hungry Leaf |
| 3/1/16 |
"How to approach the workup of suspected autoimmune disease" |
Lisa Criscione-Schreiber |
12:00 |
Domino's |
| 3/2/16 |
MKSAP Rheum & Amy Jones Feagin Leadership |
|
12:00 | Mediterra |
| 3/3/16 |
IM-ED Combined Conference: ETOH Withdrawl |
Brian Wasserman & Sarah Rivelli |
12:00/DN 2001 |
Subway |
| 3/4/16 |
Chair's Conference |
12:00 | Nosh |
From the Residency Office
Fellowship Program Info Sessions
Gastroenterology Fellowship Program
Monday, March 7th at 5:00pm in the Tyor Conference Room located in the GI Administrative Suite.
Hem-Onc Fellowship Program
March 1, 2016 4:00-5:00 PM. Room 405 Mudd (Conference Room). Pizza and drinks will be provided.
General Internal Medicine Career Night
General Internal Medicine Career Night
Interested in a career in General Internal Medicine?
Thinking about primary care medicine or hospitalist medicine?
Envision working in academics, research, Quality Improvement
or a combination?
Come to Gen Med Career Night
Tuesday March 15, 2016
6:30-8:30pm
Gen Med Resident Library
Dinner from Nosh
Come ask questions for our panelists about their path and journey:
Kevin Shah, Claire Kappa, Bruce Peyser, Sharon Rubin, David Edelman, Sonal Patel, Lance Teagen, Gene Odone, David Gallagher and Daniella Zipkin
Please RSVP to Sharon.rubin@dm.duke.edu by March 11, 2016
Teaching and Leading EBM: A Workshop for Educators and Champions of Evidence-Based-Medicine
Registration is now open!
Teaching and Leading EBM: A Workshop for Educators and Champions of Evidence-Based-Medicine
Duke Medicine, Durham NC
April 12-15, 2016
http://sites.duke.edu/ebmworkshop
This workshop focuses not only on learning EBM skills, but also on teaching EBM. Previous participants have included rising chief residents, faculty charged with developing an EBM curriculum, librarians, and other clinicians and faculty passionate about applying the best evidence to patient care. The program includes large group sessions in the morning, then supportive, small group, learner-driven sessions for the rest of the day.
The workshop will take place on the Duke Medicine campus in the new Trent Semans Center for Health Education and the Duke Medicine Pavilion.
Workshop Objectives:
Train leaders in medicine to facilitate evidence-based clinical practice in their teaching and practice settings.
Practice the skills involved in evidence-based medicine including clinical question formation and acquisition of medical evidence from the literature.
Review and develop critical appraisal skills and application of available evidence to patient care and medical education.
Develop skills in teaching EBM in both large and small group settings.
Provide interactive experience with a variety of evidence-based resources guided by faculty with expertise in evidence-based practice.
Please contact Megan von Isenburg (megan.vonisenburg@duke.edu) or Laura Huffman (laura.huffman@dm.duke.edu) with any questions.
11th Annual Duke Health Patient Safety and Quality Conference
REGISTRATION NOW OPEN: 11th Annual Duke Health Patient Safety and Quality Conference
11th Annual Duke Health Patient Safety and Quality Conference
Thursday, March 10, 2016
Durham Convention Center
301 West Morgan Street, Durham, NC
Onsite registration/check-in begins at 7:00 AM
Conference program is from 8:00 AM-4:30 PM
Register online today!
Book Club Survey
If you haven't been to one of our events yet, please support the Dept of Medicine book club project by taking a quick moment to fill out the survey below! Your participation is totally voluntary and anonymous, and the questions only takes ~2 minutes. You may remember filling this out before -- if you have, try to use the same identifier you used last time (if you can't find it, just make up a new one).
Here's the link: https://duke.qualtrics.com/SE/?SID=SV_bfJqGFkA6HScRq5
Feel free to email Laura.Caputo@duke.edu if you have any questions. Thanks so much for your participation!
Teaching and Leading EBM Scholarships
Three scholarships are available for the nationally-recognized “Teaching and Leading EBM” Workshop, which will be held at Duke Medicine from April 12 – 15, 2016. These scholarships are funded by a GME Innovations project and are reserved for residents, fellows and junior faculty who can bring EBM back to Duke residency programs. The workshop focuses not only on practicing EBM, but also on teaching EBM, making it an ideal educational opportunity for rising chief residents or others involved in teaching and the education of your residents.
We invite you to apply or to identify a member of your program to attend the workshop.
Scholarship recipients will be expected to create an educational deliverable on EBM for their programs. Deliverables could be a live session or physical / online materials. After completion of the workshop and deliverable, recipients will be required to complete a short report detailing their contribution to their programs.
Selection will be based, in part, on how participants will use the skills gained in the workshop to foster EBM in your program.
Read more about the Duke EBM Workshop here - http://sites.duke.edu/ebmworkshop/. Please contact Megan von Isenburg at megan.vonisenburg@duke.edu or 919.660.1131 with any questions.
Apply online at http://tinyurl.com/dukeebm2016
Opportunities for Wellness
Feeling down? Need to talk to someone?
All trainees at Duke have FREE access to Personal Assistance Services (PAS), which is the faculty/employee assistance program of Duke University. The staff of licensed professionals offer confidential assessment, short-term counseling, and referrals to help resolve a range of personal, work, and family problems. PAS services are available free of charge to Duke faculty and staff, and their immediate family members. An appointment to meet with a PAS counselor may be arranged by calling the PAS office at 919-416-1PAS (919-416-1727), Monday through Friday between 8:00 A.M. and 5:00 P.M. For assistance after hours, residents and fellows can call the Blood and Body Fluid Hotline (115 inside DUH, 919-684-1115 outside) for referral to behavioral health resources. Another resource is Duke Outpatient Psychiatry Referrals at (919) 684-0100 or 1-888-ASK-DUKE.
https://www.hr.duke.edu/pas/
Upcoming Dates and Events
March 2 - JAR Networking Event
March 5 - UNC vs Duke
March 18 - Match Day Celebration
April 29 -Charity Auction
Useful links
GME Mistreatment Reporting Site
https://intranet.dm.duke.edu/influenza/SitePages/Home.aspx
http://duke.exitcareoncall.com/
Main Internal Medicine Residency website
Main Curriculum website
Department of Medicine
Confidential Comment Line Note: ALL submissions are strictly confidential unless you chose to complete the optional section requesting a response
Opportunities
www.bidmc.org/CentersandDepartments/Departments/BIDHC
http://www.careermd.com/employers/latestbulletins.aspx