From the Director

When did it get to be the second week of March? Get ready for the shortest “24+4” of the year with daylight savings time coming up this weekend. Hopefully some of you who are on call on Saturday night also got the “longest day of the year” this fall :>. Super excited for it to be light out when leaving work. Thanks to Lynsey and Madi for setting up our night out to watch the Duke-UNC game. Regardless of the game outcome, fun night had by all of us.
And, of course, a HUGE thank you to the chiefs, JARs, SARs and office for the background planning for one of the greatest Duke traditions of all time, INTERN DAY OFF! AJ Blood was in on the secret and planned a fantastic day for his class, and we were all very happy to be here while our interns got a much needed surprise break. Also thanks to Murat Arcasoy for hosting a party at his house for his advisees – word is that everyone had a wonderful time.
Kudos to Kevin Friede for his (perennial) willingness to help out with a colleague in need, to Rajiv “MacGyver” Agarwal from Lauren Ring for helping her to escape the loading dock (See attached photos. And remember this for trivia bowl next year), to John Musgrove from Liz Hankollari for his night float H and P’s, to Landon Brown and Ashley Naughton from Amy Lee for great work on their first week back on Gen Med, and to our outgoing ACRs Ryan Jessee, Emily Ray and Ashley Bock. Welcome to Bassem Matta, Adva Eisenberg and Steph Giattino, our current ACRs.

Looking forward to Match week, as well as March Madness. We will be getting our brackets out once they are announced – stay tuned.
JARS, and any SARS applying to fellowship – please schedule your meeting with me (via Madi) so we can discuss your personal statement, CV, choices, etc. Many of the SARs are trying to reach out as well – Jon Hansen is coordinating a cardiology info night, so stay tuned (and thanks Jon!)
Today, Dr. Klotman sent out information about the Duke OutList, the result of long term efforts from DukeMed Pride and other members of our Duke family. I had the opportunity to meet with the leaders of DukeMed Pride last year, and am really happy to see their work come to fruition.
To recap, The School of Medicine’s student LGBTQ & Allies group, DukeMed Pride, is initiating an institution-wide project with the support of the Office of Culture, Engagement, and Impact, and the Duke Medicine Sexual & Gender Diversity Council. The project is an OutList, a list of healthcare providers who are openly gay, lesbian, bisexual, transgender or consider themselves to be allies.
OutLists exist at several other institutions, such as Harvard Medical School, Johns Hopkins, the University of Pennsylvania, and UCSF, and serve as a way for LGBTQ health professional students to receive mentorship and guidance while also creating an open, affirming institutional culture.
The Duke Medicine OutList will serve a role in medical education, patient care, and community among faculty and housestaff. An OutList also conveys an important message to talented people outside of Duke who seek to join a top-notch institution that fosters a climate of inclusion and sense of belonging for everyone.
We encourage any physician or housestaff who supports and advocates for marginalized sexual and gender diverse peoples to add your name to the Duke Medicine OutList.
Complete the DukeMed OutList Survey if you wish to be listed.
This week’s pubmed from the program goes to alum Hany Elmariah for his recent publication in the American Journal of Medical Quality. The Burden of Burnout: An Assessment of Burnout
Among Internal Medicine Residents After the 2011 Duty Hour Changes Hany Elmariah, MD, MS1, Samantha Thomas, MB2, Joel C. Boggan, MD, MPH1,3, Aimee Zaas, MD, MHS1, and Jonathan Bae, MD1 . DOI: 10.1177/1062860615625802
Have a great week!
Go Duke!
Aimee


What Did I Read This Week?
Submitted by Armando Bedoya, MD
Assessment of Clinical Criteria for Sepsis For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3)
JAMA. 2016;315(8):762-774. doi:10.1001/jama.2016.0288
Recently, the Society of Critical Care Medicine and the European Society of Intensive Care Medicine convened the Third International Consensus Task Force (Sepsis-3) to examine the definition of “Sepsis.” The definition had not been changed since 2001 and several advances have been made since. The reported incidence of sepsis is increasing likely reflecting an aging populations with more comorbidities, greater recognition, and, in some cases, reimbursement-favorable coding. To give you perception, In North Carolina alone the incidence exceeded 50,000 in 2015. Sepsis has also been targeted by the Centers of Medicare and Medicaid Services (CMS) for its Value Based Purchasing program.
As one can imagine, changing the definition has wide-ranging implications and it will likely take years for healthcare to change its practices. Furthermore, Sepsis-3 has also only been endorsed by the Society of Critical Care Medicine, the American Thoracic Society, and the American Association of Critical Care Nurses. It has not been endorsed by the American College of Chest Physicians, the Infectious Disease Society of America, any of the Emergency Medicine societies, or any of the hospital medicine societies. It is difficult to call this a consensus guideline without support from other organizations.
There are two original investigations in last week’s issue as well as the formal special communication from the task force. I urge you to read all three but we will address the first article today.
The holy grail in sepsis is to validate a clinical criterion which can identify early patients with suspected infection who are risk for sepsis. As we all are aware, every hour of delayed treatment mortality rises by ~7.6%. Early implementation of the Sepsis Care Bundles has shown a 36-40% reduction in the odds of a patient with sepsis dying in the hospital. With this information in mind, the taskforce subsequently designed a large retrospective cohort using adult encounters with suspected infections. These were hospital encounters (older than 18) were gathered from various datasets ranging from 2008-2013. The first episode of suspected infection was identified as the combination of antibiotics and body fluid cultures.
They determined clinical criteria for sepsis based upon existing measures, which included the systemic inflammatory response syndrome (SIRS) criteria; the Sequential Organ Failure Assessment (SOFA) score; and the Logistic Organ Dysfunction System (LODS) score, a weighted organ dysfunction score. Scores were calculated for the time window from 48 hours before to 24 hours after the onset of infection. Subsequently using multivariable logistic regression and Bayesian Statistics the quick Sequential Organ Failure Assessment (qSOFA) was developed.
Variables are Below:
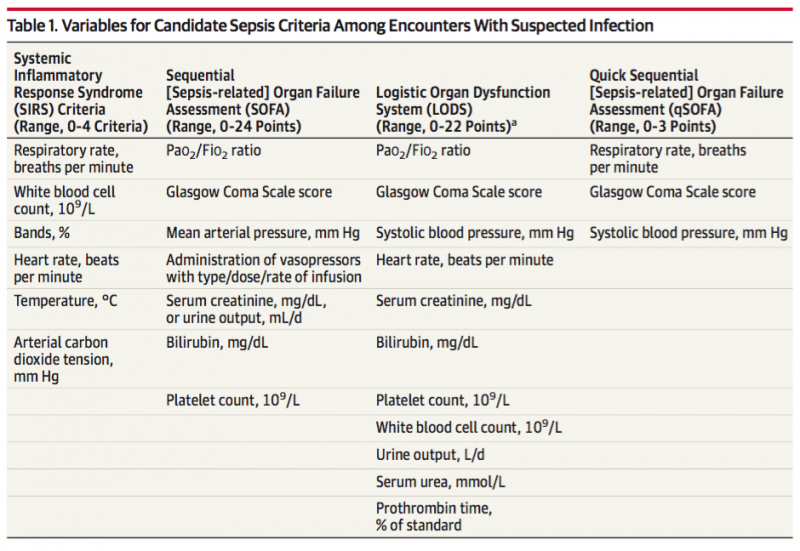
As you have noticed, the serum lactate is not part of any of the clinical criteria models nor part of the qSOFA. Per the authors: “Lactate did not meet pre-specified statistical thresholds for inclusion in qSOFA…[and] The qSOFA consistently identified higher risk encounters even at varying serum lactate levels”
Criterion validity was assessed using the predictive validity of the candidate criteria with outcomes (primary outcome: in-hospital mortality; secondary outcome: in-hospital mortality or intensive care unit [ICU] length of stay ≥3 days). Analyses were separately performed in ICU encounters and non-ICU encounters at the onset of infection.
Results are below:
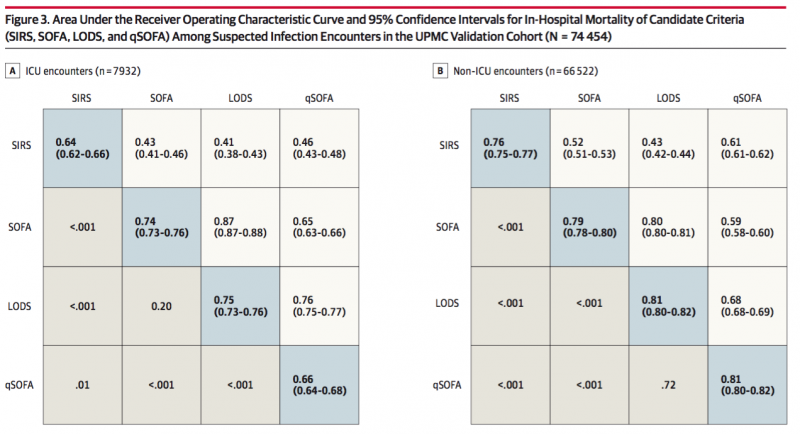
Among encounters with suspected infection in the ICU, SOFA and LODS had statistically greater predictive validity compared with SIRS criteria. Outside of the ICU, the qSOFA had statistically greater predictive validity than the SOFA score. Thus, the task force recommended use of a SOFA score of 2 points or more in encounters with infection as criteria for sepsis and use of qSOFA in non-ICU settings to consider the possibility of sepsis.
Things to keep in mind:
The SOFA score is an illness-severity score which may be used to predict the mortality of any critically ill patient. qSOFA was also designed to predict mortality (albeit within the context of a cohort of patients with suspected infection). Thus, qSOFA and SOFA are predictors of mortality; they are not tests of sepsis. Furthermore, SIRS and qSOFA have relatively similar AUROC (see above) indicating they have similar overall test performance. This is discussed in one of the three other articles but these articles lead up to the idea that the qSOFA will be the screening test and SOFA will be the definitive test. Combining qSOFA and SOFA scores is not evidence-based among patients and the combined performance of {qSOFA + SOFA} for mortality is also not reported.
Perhaps the greatest caveat to the qSOFA and the SOFA is that no organ dysfunction measurements evaluated in the two investigations can distinguish between chronic and acute organ dysfunction. Thus the patient with dementia will automatically arrive with an elevated qSOFA score but may not be as likely to have sepsis.
QI CORNER
Happy March everyone! We have a PSQC meeting this Thursday from 5:30-6:30pm and would love to have your input. Come join us in the med res library for dinner and hear about the ongoing QI projects.
In addition, anyone interested in brainstorming next year's SharePoint yearlong QI project with the ACLT group - please email me so we can put a dinner together.
CLINIC CORNER

by Lynn Bowlby, MD
Next time pictures like Sharon does for Pickett Road!
The news from the DOC!
We can show you the empty medical records space that will likely be ours! The space is in the back near Dr Westman's clinical area, and the break room.
This new space will help us with our growth, including our 2 new Counselor/MSW Ashley and Joy. They started in the past 2 weeks, and you will see them stationed near you in clinic. Like Jan, they are for on the spot counseling and mental illness help..they put their name and location on the big white boards in clinic or nursing can help you find them. Just do a warm hand off, and they will work with the pt right then and there. Awesome, and they are terrific.
ICD 10 billing...as you know we switched in October from ICD 9, and payors have given us a waiver of sorts..but that will likely change as payors start to deny codes that are not specific. So when ever possible, use as specific a code as possible for your visits so we get paid!
Do you know the leadership staff at DOC? Lisa Lowe-Hall, admin director, Candi , Clinic Operations Dir (nursing leader) and Jodi Hewitt, temp nurse manager until at least April. We continue to look for a perm. nurs manager, not that we could replace Gina.
Jodi is from Fam Med, Pickens and has been great.
There are several temp nursing staff to help as well. Connie is not at DOC now. There should be a new front desk staff member soon, and Johnetta is going full time to anther clinic (Fin Care Counselor).
Lab followup....all patients should be notified about their labs..normal or not..phone call, letter, mychart message. your nursing team can help.
If you don't know who your nursing team members are..ask , or look on BB in consult room for Care Team map, 3 colors for the 3 Stead teams. Letters should be routed to Carolyn Lawrence to send out. We can help you if you don't know how to do that..
Remember possible pregnancy when doing meds or tests...any woman under 40, just have that possibility when making your plans.
CT followup needed for nodule etc? The best way to note that is in the problem list...in the overview section under the problem , note when followup needed. We often are the owners of those plans...
DOC Redesign 2 is underway! Will roll out Intensive Primary Care in July..what is that? We are expanding our ability to treat pts for their acute illness at the DOC as well as better manage their chronic illness....like HomeBASE but for severe physical illness, not mental illness. Watch for more info!
The Maestro Concierge folks will be around , about once a week at the DOC, save your Maestro questions for them!
you can always email them as well, David Claxton.
Continue to remember Heather Hoecker, our new PA and Julia Gamble NP for your pts..some pts would be great to be paired with them or you for their visits to limit the number of providers seeing a pt. so that is a great option that is not your PP.
DM and HTN groups! and Erik, PT,
just write on the followup line in Maestro.
Thanks all for your hard work at the DOC!
Lynn and team!
From the Chief Residents
Grand Rounds
Friday, March 11 - Nephrology, Dr. Julia Scialla
Noon Conference
| Date | Topic | Lecturer | Time | Vendor |
| 3/7/16 |
MKSAP ID |
Chiefs |
12:00/2002 | Bullocks |
| 3/8/16 |
MED-PEDS Combined: Med-Peds SAR Talk |
Drs Bostwick and Turner |
12:00/2002 |
Cosmic Cantina |
| 3/9/16 |
Bugs and Drugs/ 5 minutes taken by COPD group (Annie, Luke, and Landon) |
Chris Hostler |
12:00 | China King |
| 3/10/16 |
TB |
Jason Stout |
12:00 |
Chick Fil A |
| 3/11/16 |
Chair's Conference |
12:00 | Firehouse Subs |
From the Residency Office
Fellowship Program Info Sessions
Gastroenterology Fellowship Program
Monday, March 7th at 5:00pm in the Tyor Conference Room located in the GI Administrative Suite.
GME Residency Council Updates
Inter-program social activity update:
Please join us at Tyler's - Wednesday, March 9 at 6:30 PM - All GME Residency Programs are encouraged to attend!
2016 NANCY WEAVER EMERSON LECTURESHIP
"A Singular Intimacy: Connecting the Bridge Between Caregiver and Patient"
Thursday, April 7, 2016 5:45 p.m. Great Hall, Trent Semans Center
Please see the attachment below for more information.
Charity Auction 2016 -Save the Date!
The Internal Medicine Residency program Charity Auction, benefiting Senior PharmAssist will take place Friday, April 29th, 2016 @ 7:00 p.m. at Motorco in Durham! Tickets will go on sale the first week in April. We look forward to seeing you there.
General Internal Medicine Career Night
General Internal Medicine Career Night
Interested in a career in General Internal Medicine?
Thinking about primary care medicine or hospitalist medicine?
Envision working in academics, research, Quality Improvement
or a combination?
Come to Gen Med Career Night
Tuesday March 15, 2016
6:30-8:30pm
Gen Med Resident Library
Dinner from Nosh
Come ask questions for our panelists about their path and journey:
Kevin Shah, Claire Kappa, Bruce Peyser, Sharon Rubin, David Edelman, Sonal Patel, Lance Teagen, Gene Odone, David Gallagher and Daniella Zipkin
Please RSVP to Sharon.rubin@dm.duke.edu by March 11, 2016
Teaching and Leading EBM: A Workshop for Educators and Champions of Evidence-Based-Medicine
Registration is now open!
Teaching and Leading EBM: A Workshop for Educators and Champions of Evidence-Based-Medicine
Duke Medicine, Durham NC
April 12-15, 2016
http://sites.duke.edu/ebmworkshop
This workshop focuses not only on learning EBM skills, but also on teaching EBM. Previous participants have included rising chief residents, faculty charged with developing an EBM curriculum, librarians, and other clinicians and faculty passionate about applying the best evidence to patient care. The program includes large group sessions in the morning, then supportive, small group, learner-driven sessions for the rest of the day.
The workshop will take place on the Duke Medicine campus in the new Trent Semans Center for Health Education and the Duke Medicine Pavilion.
Workshop Objectives:
Train leaders in medicine to facilitate evidence-based clinical practice in their teaching and practice settings.
Practice the skills involved in evidence-based medicine including clinical question formation and acquisition of medical evidence from the literature.
Review and develop critical appraisal skills and application of available evidence to patient care and medical education.
Develop skills in teaching EBM in both large and small group settings.
Provide interactive experience with a variety of evidence-based resources guided by faculty with expertise in evidence-based practice.
Please contact Megan von Isenburg (megan.vonisenburg@duke.edu) or Laura Huffman (laura.huffman@dm.duke.edu) with any questions.
Book Club Survey
If you haven't been to one of our events yet, please support the Dept of Medicine book club project by taking a quick moment to fill out the survey below! Your participation is totally voluntary and anonymous, and the questions only takes ~2 minutes. You may remember filling this out before -- if you have, try to use the same identifier you used last time (if you can't find it, just make up a new one).
Here's the link: https://duke.qualtrics.com/SE/?SID=SV_bfJqGFkA6HScRq5
Feel free to email Laura.Caputo@duke.edu if you have any questions. Thanks so much for your participation!
Duke Division of Hematology Newsletter - March 2016
See link below for PDF.
Opportunities for Wellness
Feeling down? Need to talk to someone?
All trainees at Duke have FREE access to Personal Assistance Services (PAS), which is the faculty/employee assistance program of Duke University. The staff of licensed professionals offer confidential assessment, short-term counseling, and referrals to help resolve a range of personal, work, and family problems. PAS services are available free of charge to Duke faculty and staff, and their immediate family members. An appointment to meet with a PAS counselor may be arranged by calling the PAS office at 919-416-1PAS (919-416-1727), Monday through Friday between 8:00 A.M. and 5:00 P.M. For assistance after hours, residents and fellows can call the Blood and Body Fluid Hotline (115 inside DUH, 919-684-1115 outside) for referral to behavioral health resources. Another resource is Duke Outpatient Psychiatry Referrals at (919) 684-0100 or 1-888-ASK-DUKE.
https://www.hr.duke.edu/pas/
Upcoming Dates and Events
March 18 - Match Day Celebration
April 29 -Charity Auction
May 19 - Resident Research Night
Useful links
GME Mistreatment Reporting Site
https://intranet.dm.duke.edu/influenza/SitePages/Home.aspx
http://duke.exitcareoncall.com/
Main Internal Medicine Residency website
Main Curriculum website
Department of Medicine
Confidential Comment Line Note: ALL submissions are strictly confidential unless you chose to complete the optional section requesting a response
Opportunities
www.bidmc.org/CentersandDepartments/Departments/BIDHC
http://www.careermd.com/employers/latestbulletins.aspx