
Building an Age-Friendly Health System
In nearly every specialty area of medicine, providers are seeing an increasingly disproportionate number of older adult patients. As of 2021, there were more than 46 million people aged 65 and older in the U.S. and by 2050, that number is expected to grow to almost 90 million, according to census data.
Duke University Health System is working head on to meet the challenge by participating in the Age-Friendly Health System (AFHS) movement, a systemic-change framework under which health systems across the country can improve and personalize their care of older adults through recognition as being Committed to Care Excellence by the Institute for Healthcare Improvement (IHI).
The goals for Duke are to integrate AFHS protocols and practices across all hospitals and outpatient clinics as part of the health system’s strategic plan for excellence in clinical care and to create an educational pathway for Duke learners. The foundation for the Age-Friendly system is being laid at Duke Regional Hospital (DRH), a hub of innovation in caring for older adults where, on any given day, there are over 100 admitted patients over the age of 65.
With more geriatric patients getting surgery and being hospitalized than ever before, and more people coming to North Carolina to retire, the need to provide better evidence-based health care is growing alongside the aging population, which is more likely to have complex medical issues and a greater need to be in the hospital or interact with the health care system.
“We need to do better about taking care of older adults, preventing frailty, weakness, malnutrition and other avoidable issues so that they can stay healthy and not need us so much,” says Serena Wong, DO, an assistant professor in the division of Geriatrics who is leading the AFHS program development at DRH. “Using the simple Age-Friendly framework and applying it to each patient can make a big impact on their independence, their quality of life and hopefully reduce their need to be hospitalized in the first place.”
Wong also points out a critical need for learners across all disciplines to be trained in some basic geriatric framework of patient care, which is essential in understanding how to prevent the “hazards of hospitalization” such as delirium and medication interactions, events that impact many older adults.
“When you think about how many of our future doctors will be taking care of older adults, that’s basically everyone unless you're a pediatrician,” Wong says. “So, it's important for most of our future providers and nurses and other healthcare team members to have some basic knowledge about geriatrics.”
Providers can provide much better care if the whole team is working from the same foundational understanding, notes Heidi White, MD, clinical vice-chief of the division of Geriatrics and chair of the Steering Committee of the Geriatrics Operational Plan for the Duke University Health System.
“When we talk about an Age-friendly Health System, we're talking about everybody in the system having some knowledge and understanding of how to provide impactful care for older adults,” White says. “Providers are actually only one member of the team and, from the patient's perspective, every team member is important whether it's the person at the front desk, the person cleaning the room, the nurse or the provider. We, as providers, need to be more cognizant of the fact that we are one cog in the wheel.”
The AFHS framework itself serves as teaching tool. It is based on tiered system called the Four Ms that guide all care of older patients wherever and whenever they come into contact with the health system. The intent for Duke is to incorporate the 4Ms into existing care, which is achieved primarily through redeploying existing system resources.
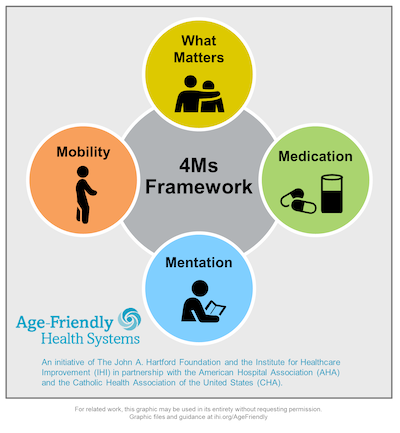
The Four Ms
- What Matters: Know and align care with each older adult’s specific health outcome goals and care preferences across settings of care, including end-of-life care
- Medication: Use age-friendly medication that does not interfere with What Matters to the older adult, Mobility or Mentation across care settings
- Mentation: Prevent, identify, treat and manage dementia, depression, and delirium across settings of care
- Mobility: Ensure that older adults move safely every day in order to maintain function and do What Matters.
“The IHI 4Ms framework is a wonderful way for learners to identify modifiable risk factors, and better align their care with the patient’s goals,” says Cathleen Colón-Emeric, MD, chief of the division of Geriatrics. “I believe that it also fosters more meaningful and rewarding interactions with patients because learners must step back and see patient as a whole person rather than as someone with a single disease of interest in the moment.”
The DRH Hub
At DRH, an interprofessional AFHS steering committee is developing 4Ms processes and testing their implementation on two medical units. The team’s goal is to expand to all medical and surgical units at DRH in the next 1-2 years.
DRH is addressing Mentation by screening for delirium throughout the hospital with nurses implementing a care plan to reduce delirium with all of their patients regardless of age. Nurses also screen for mobility deficits at least once per shift, and patients are being mobilized at least twice a day.
Medication efforts in progress include the use of a system-wide electronic health record process that automatically adjusts dosing for age to reduce exposure to high risk medications as they are ordered. Teams are also thinking about ways to better communicate recommendations about high-risk medications to outpatient providers, who have more longitudinal relationships with patients and may be better equipped to guide medication changes in the long term.
For What Matters Most, DRH is promoting interdisciplinary care and engaging multiple groups in the healthcare team to engage patients in determining their health care goals. One role of case managers, for example, is to support patients during discharge planning, which may include transition to a skilled nursing facility. This discharge plan may help the patient regain strength and mobility, and better equip them to return home, which is What Matters Most to many of our older patients. For physical and occupational therapists, asking patients What Matters Most to them can help them create meaningful therapeutic goals with patients, better tailor therapy plans to each patient’s needs and priorities, and motivate patients to participate to the best of their abilities.
Older patients are not just patients who have more birthday candles on the cake, Wong adds; they are moving differently and have different needs, priorities and goals. “For younger folks, we always assume everyone wants to live longer and be healthier,” she says. “But as people get older, we start to think about what's really in line with their personal goals.
“Everybody wants the very best diagnosis of treatment but we also have to put that into the context of what matters to them, life expectancy, their overall prognosis,” White says. “Older adults really do have a different perspective on what matters to them, and it's not just the highest quality, best technology, savvy treatment that is important to them. They care about having the strength, balance and breath to do their own grocery shopping or attend an upcoming family wedding. Making sure their medical work up and treatment accommodates and prioritizes their specific goals is what Age Friendly is about. ”
IHI Age-Friendly recognition is one of many geriatric innovations underway at DRH, which earned Bronze-Level Geriatrics Emergency Department Accreditation (GEDA) in January 2020 in recognition of ED’s protocols that meet the needs of older patients. One interdisciplinary protocol for hip-fracture patients, for example, provides alternative non-opioid pain management and a faster transition to the operating room for those who need surgery. Such efforts help reduce incidents of complications such as hospital-acquired delirium and falls.
An increasing number of nurses and CNAs are training to become Geriatric Resource Nurses (GRNs) or Geriatric Patient Care Advocates (GPCAs) through programs offered by the Duke Center of Geriatric Nursing Excellence (CGNE) in collaboration with DUHS Clinical Education and Professional Development. GRNs and GPCAs have contributed immensely to the successful roll out of mobility and delirium redesign at all three Duke hospitals.
DRH’s age-friendly journey started in 2019 with a recognition of AFHS participation, but the goal will not be fully achieved until the entire system can become age-friendly for all individuals over the age of 65. “That’s probably still years away; we are working diligently right now to achieve IHI AFHS recognition as committed to care excellence, at DRH,” she says. “But there is an element that we're working and talking about Age-Friendly in everything we do now and much of the work within disciplines and departments is being incorporated beyond the walls of DRH.”