by Scott Huler
Dr. Perfect has heard them all.
John Perfect, MD, professor of medicine (Infectious Diseases) and associate professor in molecular genetics and microbiology, focuses on medical mycology—the troubles fungi cause other organisms, especially people.
He recently published a paper, in the journal mBio, with David Tobin, PhD, assistant professor of molecular genetics and microbiology, which got a lot of attention. Addressing Cryptococcal meningitis, the paper described using zebrafish to learn how the fungus Cryptococcus crosses the blood-brain barrier to cause human disease. Partially because the paper linked to a stunning video of fluorescent, bright red fungi moving their way through the host into its brain like something out of a sci-fi movie, the paper has received enormous attention.
So, of course, according to Perfect, the video didn’t go viral.
It went fungal.
Welcome to the world of mycology jokes.
Perfect remembers his life-changing meeting with H99, the strain of Cryptococcus he still uses in research, in 1978, at 11 p.m. as he worked in his lab—on Feb. 14, Valentine’s Day. It’s not exactly “the Germans wore grey, you wore blue,” but his wife does sometimes claim he fell in love with the fungus, not her. In fact, the fungus is encapsulated in a shell of polysaccharides—it’s actually sugar-coated—so with her husband sharing sweets on Valentine’s Day with a fungus it’s hard to blame her for the joke.
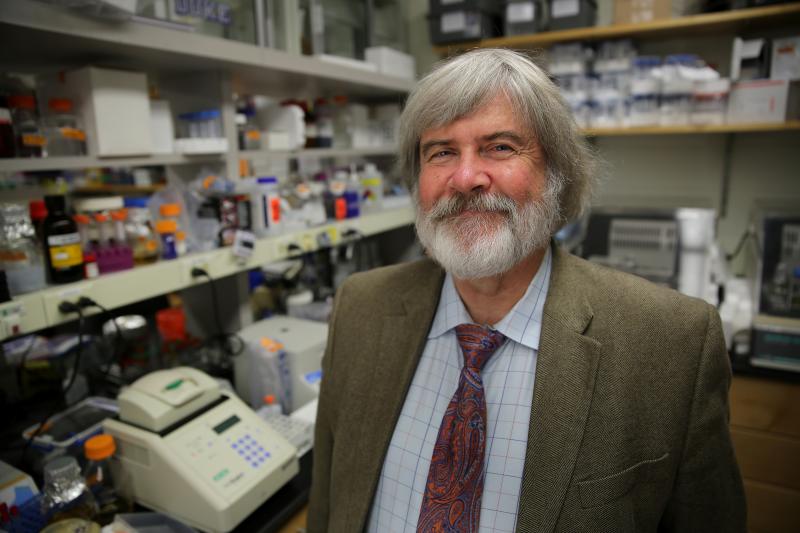
Which Perfect, who favors paisley ties and tends to grin from beneath a Warholian shock of white hair, cheerfully does. In fact, he titled one of his own papers “Cryptococcus neoformans: a sugar-coated killer with designer genes.”
“Cryptococcus neoformans, or Cryptococcus gattii, cryptococcal disease, is the most common cause of central nervous infection that we see at Duke and many parts in the southeastern part of the US,” Perfect explains. You and pretty much everybody breathe in little Cryptococcus spores constantly, especially in the Southeast, where it lives in the dust, in the trees, the pigeon guano. But unless you’re immunosuppressed, the fungus doesn’t cause you any trouble. If you are immunosuppressed, however—perhaps you’re taking corticosteroids or have had a transplant—you may be in trouble.
Perfect estimates a million cases of cryptococcal disease per year, with 600,000 deaths, most of them in sub-Saharan Africa where AIDS causes widespread immunosuppression. People can develop respiratory symptoms, like pneumonia; if the pathogen crosses the blood-brain barrier, the infection progresses to terrible, long-lasting headaches and sometimes fever. There can even be other neurological signs; cryptococcus can actually cause dementia.
The problem is, even though we understand that Cryptococcal disease occurs in the immunosuppressed, we don’t know quite how the fungus sneaks through the blood-brain barrier.
“There are about 1.6 million fungi in the world,” said Perfect. “About 15 consistently cause disease in humans.”
What makes Cryptococcus so special?
We know how to look for answers to questions like that, too, and Perfect has spent decades at it.
“It’s been sequenced,” said Perfect of his lifelong companion, Cryptococcus H99. “We can knock genes out, we can put genes back in.”
You can mess with the genes, inject the organism with the manipulated genes into model systems, and see how they do.
Oh yeah, model systems—that’s a key part of the story. You can do all kinds of things to a pathogen in a test tube.
“But that’s a test tube,” Perfect says. “Not a mammalian host.”

Enter the zebrafish.
Wait—didn’t Perfect say “mammalian host”? And isn’t the zebrafish a fish?
Why, yes. Which is part of what makes the mBio paper so remarkable. Larger animal models—rabbits or mice, for example—do a great job modeling disease process that’s transferrable to people. The problem is they’re big and expensive and they take up lots of space and a long time to use.
So say hello to David Tobin, who spends much of his time at Duke infecting zebrafish with stuff—including, for example, tuberculosis. And if you are about to point out that zebrafish don’t have lungs, you’re getting the point. The zebrafish may not have lungs, but it shares 70 percent of its DNA and anatomy with humans, so it provides a great model system for testing the pathways of infection, even in mammals.
That is, the zebrafish, tiny and easy to raise, provides a far cheaper and faster model than mice and rabbits for understanding disease process. What would take months with mammals takes weeks with zebrafish.
“What Stefan Oehlers and Jenny Tenor, from John’s lab, were able to show,” Tobin said, “was that you were now able to use the fish to model that step of crossing the blood-brain barrier.”
And when he says “show” he means that literally.
Zebrafish, as larvae and even as early adults, are transparent. You label different cells in the host—you introduce certain molecules that attach to specific areas in the host and glow when you look at them with a fluorescence microscope. In the video from Perfect and Tobin’s paper, you can watch as macrophages, fluorescing in blue, attack the Cryptococcus, fluorescing in red. Watching the pathogen attack the subject’s brain is kind of like sci-fi, but Tobin keeps his eyes on the prize: figuring out how the Cryptococcus crosses that blood-brain barrier.
“Is the crossing happening within an infected macrophage? We actually tried fairly hard for this paper to look at that question and we haven’t been able to answer it.”
That is, macrophages, which try to fight the infection, themselves get infected, and then…well, nobody’s quite sure; says Tobin, “We can manipulate the fish and remove macrophages altogether, and the infection gets much worse.” So the macrophages aren’t the problem, though they’re part of the process. “That’s certainly something we are going to keep looking at.”
Looking together, Perfect points out, expressing gratitude for “the ability to interact with other scientists and the collaborative nature we have here at Duke.” In fact, Tobin and Perfect received an Integrated Research 2012 grant from the Department of Medicine to help get their collaboration started.
Tobin said they also checked certain genetically manipulated strains of Cryptococcus that had proven unable to cross the barrier in mammals—and they proved just as compromised for virulence in the zebrafish. “That’s reassuring that the biology is working similarly in mammals and zebrafish,” he said, further strengthening the zebrafish’s utility as a model.
“It’s a very attractive model,” said Perfect.
[video:https://youtu.be/tNOxUjFe4vY]
Scott Huler is a writer based in Raleigh, North Carolina. Learn more about him at scotthuler.com.