Core Program Curricula
Evidence-based Medicine in Geriatrics - Director: Dr. Mamata Yanamadala
In this 8-part series of interactive didactics with case applications, fellows learn the practice and application of Evidence Based Medicine in geriatrics.
Quality Improvement Course - Directors: Dr. Gwendolen Buhr and Dr. Mamata Yanamadala
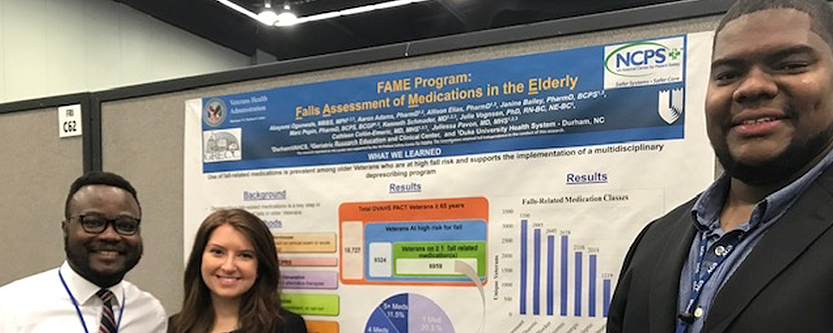
This well tested QI curriculum has been in place since 2008 and has been continuously modified to suit fellows' needs. Fellows are immersed in a half day retreat to learn QI concepts and design projects. They are coached throughout the year with frequent meetings on QI project execution. Many fellows go on to present results of their projects at the American Geriatrics Society National Meeting.
Clinical Teaching Workshop - Director: Dr. Mamata Yanamadala
This curriculum is based on the Stanford Clinical teaching skills course designed by Dr. Kelly Skeff. Five interactive sessions provide fellows with the opportunity to learn and master a variety of clinical teaching skills applicable to a variety of settings under guidance of Dr. Mamata Yanamadala.
Advance Course in Long Term Care - Directors: Dr. Heidi White and Dr. Gwendolen Buhr
Covers key topics in long term care, including medical directorship, team building, and nursing home litigation.
Palliative Care Series
Discuss key topics in palliative care, including pain management, non-pain symptom management, communication skills, psychosocial care, and understanding systems of care.
Health Equity Course - Director: Dr. Yoon Hie Kim
Geriatric medicine fellows work with Duke faculty and Durham community leaders to explore the linkages between social factors and health and the ways in which the local community responds. Participants take a closer look at Durham and the role of race and class on access and privilege in our community. Participants also examine a variety of ways in which the people of Durham have demonstrated initiative and ingenuity in identifying and addressing inequities.
Fellow Conferences
Fellows are mentored by faculty with expertise in faculty development to present to an audience of faculty, peers, and interdisciplinary learners.
In addition to Geriatric medicine fellows, conferences are attended by trainees from a variety of other programs, including geriatric nurse practitioner residents, geriatric physical and occupational therapy residents, geriatric pharmacy residents, and trainees from the internal medicine residency, making these conferences excellent multi-disciplinary learning opportunities.
Weekly Conferences
Conferences are an essential part of the Geriatric Fellowship Program. Fellows are required to attend several weekly conferences and will periodically be invited to present. In addition to Geriatric medicine fellows, conferences are attended by trainees from a variety of other programs, including our geriatric psychiatry fellows, geriatric nurse practitioner fellows, geriatric physical and occupational therapy residents, and trainees from the internal medicine residency, making these conferences excellent multi-disciplinary learning opportunities.
| Title | Topic |
|---|---|
| Geriatric Grand Rounds | Formal presentation of a major topic in Geriatrics and Gerontology. The conference includes a monthly research conference and a monthly education seminar. |
| Medicine Grand Rounds | Topics requested by members of the Department of Medicine are selected by Chief Medical Residents, Department Chair, and Continuing Medical Education representatives. |
| Weekly “Check-in” Meetings | Fellows meet with weekly with the program director and a variety of core faculty to discuss clinical cases and/or discuss logistical issues within the program. |
"There were so many research opportunities during my fellowship year that it was difficult to pick just one! I was lucky to be able to participate in both a QI project through the VA and a process evaluation for the GWEP’s outpatient Interdisciplinary Care Team (a project that involved both Duke and Durham resources). It was an interesting year."
Karen Rhea, MD, Fellowship Alumni