New translational research: Blood test can tell if antibiotics are needed
A team of infectious disease and genomics faculty in the Department of Medicine has been fine-tuning a test that can determine whether a respiratory illness is caused by infection from a virus or bacteria so that antibiotics can be more precisely prescribed. The research was published in the January 20 issue of Science Translational Medicine.
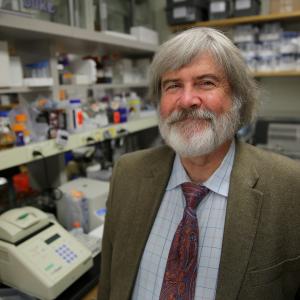
John Perfect on his research: It went fungal
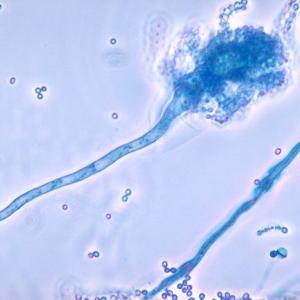
Dr. John Perfect estimates a million cases of cryptococcal disease per year, with 600,000 deaths, most of them in sub-Saharan Africa where AIDS causes widespread immunosuppression. People can develop respiratory symptoms, like pneumonia; if the pathogen crosses the blood-brain barrier, the infection progresses to terrible, long-lasting headaches and sometimes fever. There can even be other neurological signs; cryptococcus can actually cause dementia. The problem is, even though we understand that Cryptococcal disease occurs in the immunosuppressed, we don’t know quite how the fungus sneaks through the blood-brain barrier.
Bashore, Fulkerson, Klotman receive Duke Med Alumni awards
The Duke Medical Alumni Association last night honored eight highly accomplished alumni, faculty, and friends with the 2015 Distinguished Awards.
Among the recipients were three members of the Department of Medicine:
Fungal and Antifungal Therapy Symposium coming in November
The Division of Infectious Diseases will hold a Fungal Infections and Antifungal Therapy Symposium Nov. 13-14 in 131 Hanes House.
Take a look at the agenda, list of presenters and contact Michelle Harris (michelle.a.harris@dm.duke.edu) to register.
Cleaning Hospital Rooms With Chemicals, UV Rays Cuts Superbug Transmissions
A new study from Duke Medicine has found that using a combination of chemicals and UV light to clean patient rooms cut transmission of four major superbugs by a cumulative 30 percent among a specific group of patients -- those who stay overnight in a room where someone with a known positive culture or infection of a drug-resistant organism had previously been treated.
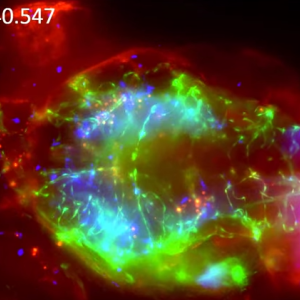
Meningitis Model Shows Infection’s Sci-Fi-Worthy Creep Into the Brain
A study led by John Perfect, MD, chief of the Division of Infectious Diseases, is using transparent fish to watch in real time as Cryptococcal meningitis takes over the brain. The resulting images are worthy of a sci-fi movie teaser, but could be valuable in disrupting the real, crippling brain infection that kills more than 600,000 people worldwide each year.
9/25/15: Grand Rounds, Research Seminar returns and two celebrations
Friday will be a particularly busy day in the Department of Medicine. The Department will host two conferences and two of its centers will mark anniversaries with seminars and celebrations.
Fowler part of collaborative research team looking at multidrug resistant bacteria
Vance Fowler, MD, MHS, professor of medicine (Infectious Diseases), is part of a research team funded by Duke Translational Medicine Institute and the Duke CTSA that is exploring the efficacy of beating back multidrug resistant bacteria by using chemical compounds known as LpxC inhibitors. These chemical compounds disrupt the formation of Lipid A in the protective membranes around Gram negative bacteria - a novel way of destroying bacteria.
Perfect awarded 5-year program project grant from NIAID
John Perfect, MD, professor of medicine and chief of the Division of Infectious Diseases, received notification today from the National Institute of Allergy and Infectious Diseases of a program project award (P01) for his proposal entitled “Transdisciplinary Program to Identify Novel Antifungal Targets and Inhibitors." This award, effective 6/25/15, will last five years and, with its cores, total $9,277,000.
Duke Human Vaccine Team awarded $5 million to study fungal fever
The Duke Human Vaccine Institute’s Vaccine and Treatment Evaluation Unit has been awarded a $5 million contract from the National Institute of Allergy and Infectious Disease to support further research on Valley Fever Pneumonia.
Valley Fever Pneumonia is caused by the fungal pathogens Coccidioides posadasii and Coccidioides immitis, which primarily live in soil. Valley Fever is endemic in certain parts of the southwestern United States, including Arizona and California.