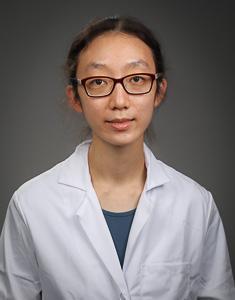
The Duke Medicine Physician-Scientist Training Program (PSTP) is designed for exceptional MD or MD/PhD candidates to seamlessly integrate clinical and research training, beginning in internship (PGY-1) and extending to the completion of a subspecialty fellowship program.
*Acceptance into PSTP includes guaranteed acceptance into the subspecialty fellowship program you interviewed with, assuming a solid clinical performance during residency.
Application to the PSTP occurs during application to Internal Medicine Residency Program. Candidates should select the PSTP two-part interview option. This allows for candidates to meet with potential research mentors, other PSTP trainees, members of the fellowship program, and divisional and departmental leadership, in addition to the standard interview day for the residency program. Our goal is to foster long-term clinical and mentoring relationships, paving the way for a career as a physician-scientist at Duke.
Initial interviews will be conducted via virtual platforms. The PSTP interview schedule is composed of two parts: morning interviews will be with categorical interviewers and afternoon interviews will be with PSTP faculty. All meetings will be conducted virtually. All interviewed candidates will be invited in February of the application season for a one-day in-person visit of Duke. Itineraries of the in-person visit will be tailored to individual applicant’s research and subspecialty interests.
Focus
The focus of the PSTP is to support trainees as they transition from medical school graduation (an MD or combined MD/PhD degree) to full-time academic appointment to achieve a career goal of becoming a successful and productive physician scientist.
Promise
Individuals choosing this track will receive a high-quality clinical training combined with a cutting-edge research training engaging broad and innovative research opportunities around the campus, ranging from bench science to healthcare policy development. PSTP Scholars will receive salary at the full ACGME level according to PGY status from internship/residency through the clinical and research years of the fellowship. (For the research years, this ACGME salary is approximately $80K/year.)
Environment
Duke offers a stellar research environment that encompasses 24 basic and clinical departments, 15 cross-pollinating Centers and Institutes, more than 30 state-of-the-art shared research facilities and cores, department-wide seminar series, school-wide initiatives, symposia and professional development programs. Career development of Duke PSTP Scholars is enhanced by school-wide entities supporting physician-scientist career development, including the Office of Physician Scientist Development (OPSD) and The Robert J. Lefkowitz Society, both of which provide additional mentoring and networking opportunities.
Program Leadership Team
Xunrong Luo, MD, PhD
Associate Director, PSTP

Christopher Holley, MD, PhD
Assistant Director, PSTP

Aimee Zaas, MD, MHS
Program Director,
Internal Medicine Residency
Each trainee accepted into the PSTP will be appointed a program advisor at the beginning of their internship year. Pairing between advisors and trainees will be based on shared research interests and compatible personalities. The role of the program advisor is to assist the trainee in constructing an individualized training plan that meets the unique needs of each trainee. The program advisors are successful physician-scientists themselves. They will meet with trainees regularly and assist trainees in making major decisions such as choice of subspecialty, research laboratory and additional didactic courses that could be taken during the research portion of a fellowship.
The majority of trainees will participate in the American Board of Internal Medicine (ABIM) Research Pathway. This pathway provides a rigorous clinical training that allows its trainees to complete the internal medicine residency in two years and to enter a subspecialty fellowship during their PGY-3. During the two years of intense clinical training, trainees will perform direct patient care (inpatient and outpatient) in one of the Duke hospitals and clinics, including the Durham VA, under direct guidance of Duke’s many talented clinical faculty members.
Two other options will also be considered and granted based on trainee’s specific needs:
- Trainees who wish to maximize their clinical training can also spend three years in clinical training as categorical internal medicine residents. Short-track in which residency training is completed in 2 years is not a requirement. Our goal is to provide the best experience for each individual in preparation for a physician-scientist career.
- Trainees who wish to maximally prepare for their research training, with careful planning, can also seek a laboratory rotation opportunity during PGY-1 or PGY-2 year if they are not participating in the 2-year clinical investigator pathway.
We have a separate match number through NRMP for PSTP distinct from the Duke Internal Medicine Categorical Residency Program. The PSTP NRMP number is 1529140C1.
Most PSTP scholars will stay at Duke for their fellowship training. The residency program and fellowship program leadership will maintain open communication during the interview process and during residency regarding fellowship match. Acceptance into PSTP includes acceptance into the subspecialty fellowship program you interviewed with, assuming a solid clinical performance during residency. For specific questions related to subspecialty fellowship, applicants are encouraged to directly contact the PSTP Associate and Assistant Directors.
The requirement of clinical fellowship training will be fulfilled per ABIM subspecialty board, which typically entails a one- or two-year intense clinical training period, followed by maintenance of a subspecialty clinic during the remainder of the fellowship training. PSTP trainees will be salaried according to PGY level through their internship/residency, as well as their clinical and research years of fellowship.
A significant advantage of being a trainee of the Duke Department of Medicine PSTP is the strength of research mentors and support available to trainees. In addition to the School of Medicine, trainees also will have the opportunity to seek mentorship from Duke faculty members from other disciplines, such as the Duke Pratt School of Engineering and the Duke Margolis Center for Health Policy. We encourage applicants to begin meeting with potential research advisors during their initial interview and to continue the process early during their clinical training years (PGY-1 up to PGY-4). We also encourage applicants to make their final choice of a research advisor in consultation with their program advisor. Each trainee must form an advising committee during the first year of their research training whose role is to guide their research direction, to assess their research progress, and to ensure their transition to independence.
Explore research in clinical Divisions of the Department of Medicine
All PSTP Scholars during their entire training period will be encouraged to integrate with other school-wide entities supporting physician-scientist career development, including the Office of Physician Scientist Development (OPSD) and The Robert J. Lefkowitz Society, in order to take advantage of additional mentoring and networking opportunities. Trainees will participate in the mandatory Ethics in Biomedical Research Course and the annual Physician-Scientist Symposium of the School of Medicine. Trainees will be encouraged to attend the annual spring AAP/ASCI/APSA joint meeting to network with physician-scientist leaders across the nation. During the final year of the program, faculty appointment as an Instructor is anticipated, based on satisfactory clinical and research progress.
During the research training period (typically PGY-3 to PGY-6), in addition to periodic meetings with the advising committee, trainees will have the options to pursue the following:
- Audit any relevant classes offered by the graduate programs of all basic science departments;
- Take one of the several grant writing classes offered by the School of Medicine;
- Earn an additional degree in Master of Science in Clinical Investigation or Master of Public Health.
Application
Individuals who are entering internship with either a combined MD/PhD degree or an MD degree with a record of intensive research experience (e.g. those with research fellowship such as a Howard Hughes or Sarnoff fellowship during medical school) are eligible to apply. Successful applicants will exhibit commitment to a career as an academic physician-scientist.
Interested applicants should apply through the Electronic Residency Application Service (ERAS) to the Duke Internal Medicine Residency Program. Applicants who are invited for an interview will receive our supplemental application, where you can indicate interest in the PSTP as well as suggestions for potential faculty you would like to meet while visiting Duke. A letter of recommendation from the applicant’s principal research mentor is mandatory. We only accept information through ERAS. For your four letters, we encourage you to select individuals who know you well, with a letter of recommendation from your principal research mentor and a departmental letter (SEL or departmental preference) being mandatory.
Please note that Duke IM residency has two separate National Resident Matching Program (NRMP) match numbers: one for the PSTP track (1529140C1) and one for the categorical track. Therefore, if an applicant is interested in ranking the Duke program(s) after they complete their interviews, please make sure to rank with the correct number(s).
Applicants to the PSTP track will be offered a two-part, one-day interview. During the first part (morning), the applicants will experience a traditional residency program interview with categorical program faculty interviewers. During the second part (afternoon), the applicants will meet with PSTP directors and potential research mentors according to their research interests. Applicants will have the opportunity for Q&A with current and former PSTP trainees at Duke. In addition, all interviewed candidates will be invited in February of the application season for a one-day in-person visit of Duke. Itineraries of the in-person visit will be tailored to individual applicant’s research and subspecialty interests. Our purpose for the second look is for you to have an in-person experience with Duke, the programs/labs you are interested in, and life in Durham in general.
PSTP Scholars
Physician-Scientist Resources at Duke
The SCI-StARR Pathway is a four-year residency with 18-months of research sponsored by the R38 Stimulating Access to Research in Residency (StARR) grant. Residents will be selected from the Departments of Medicine, Pediatrics, and Surgery to participate in this program each year. Residents who wish to pursue this pathway will apply to the program during their intern year. Learn more.
The Office of Physician-Scientist Development was established in 2018 by Dean Mary E. Klotman, MD to promote scientific engagement among physicians, trainees, and medical students. It is led by Associate Dean of Physician-Scientist Development Rasheed Gbadegesin, MD, MBBS, Associate Director of Physician-Scientist Development Gowthami Arepally, MD, and Lefkowitz Society Director Sudarshan Rajagopal, MD, PhD. The OPSD serves as a central resource for information and programming including training in grant writing, mentoring, leadership development, and funding opportunities.
This honor society elects 5-10 physician-scientists in residency or fellowship training each year from across the School of Medicine. Society members meet with each other and with physician-scientist faculty advisors to network, gain career advice, and share scientific perspectives. Society members have access to travel funds for scientific meetings and are given priority for fellowship training opportunities. Learn more.
In September 2018, Duke University School of Medicine received one of five Burroughs Wellcome Fund Physician-Scientist Institutional Awards. This program, which is led by Rasheed Gbadegesin, MD, MBBS, and a team of School of Medicine faculty, strives to enhance research excellence in laboratory-based science. Learn more.
The Office for Faculty Development and Office for Research Mentoring offer grant writing workshops, leadership development programs, professional development seminars, executive coaching, and other resources.
The Department of Medicine and School of Medicine both offer multiple internal funding opportunities, many of which are targeted to physician-scientists. Learn more.
Current T32 Training Grants by Subspecialty
Below is a complete list of The Department of Medicine's active T32 training grants by subspecialty. Applicants with specific interests in a subspecialty will be arranged to meet with the specific T32 PI/Co-PD during their interview. Should they wish, applicants can also directly contact the specific T32 PD/Co-PD to obtain more detailed information on the training grant.
| Subspecialty | Grant No. | Project Dates | Trainee Slots | PI | Co-PD |
|---|---|---|---|---|---|
| Genetics and Genomics | T32GM136627 | 7/1/20 – 6/30/25 | 4 | Allison Ashely-Koch | -- |
| Endocrinology | T32DK007012 | 7/1/19 – 6/30/29 | 4 | David D'Alessio | -- |
| Gastroenterology | T32DK007568 | 7/1/22 – 6/30/27 | 3 | Andrew Muir | Rodger Liddle |
| Hematology | T32HL007057 | 7/1/75 – 6/30/26 | 7 | Gowthami Arepally | Marilyn Telen |
| Infectious Diseases (Transplant) | T32AI100851 | 9/1/13 – 8/31/24 | 3 | Barbara Alexander | -- |
| Infectious Diseases (AIDS) | T32AI007392 | 9/1/20 – 8/31/25 | 6 | Nathan Thielman | Guido Ferrari |
| Pulmonary | T32HL160494 | 1/1/22 – 12/31/26 | 6 | Scott Palmer | Jennifer Ingram |
| Behavior and Psychology in Aging | T32AG000029 | 7/1/84 – 8/31/25 | 2 | Harvey Cohen | -- |
| Biomolecular and Tissue Engineering | T32GM144291 | 7/1/22 – 6/30/27 | 2 | Charles Gersbach | Tatiana Segura |
| Molecular Mycology and Pathogenesis | T32AI052080 | 8/1/23 – 7/31/29 | 6 | Joseph Heitman | Andrew Alspaugh |
| Viral Oncology | T32CA009111 | 7/1/80 – 1/31/25 | 4 | Micah Luftig | -- |
| Nephrology | TLDK139567 | 9/1/23 – 6/30/28 | 6 | Steven Crowley | -- |