Prognostic Value of CMR Stress Testing
Noninvasive cardiac stress testing is a cornerstone in the clinical treatment of patients with known or suspected coronary artery disease (CAD). While multiple prior reports and meta-analyses have found that cardiac MR (CMR) is more accurate for the diagnosis of CAD compared to conventional imaging methods, CMR still represents less than 0.1% of all imaging-based stress tests in the United States. The limited use of stress CMR is likely due to several factors, including the availability of good-quality CMR laboratories, exclusion of patients with implanted metal, and lack of data on patient outcome. The prognostic value of stress CMR has previously only been reported in smaller single-center studies, with limited events and short follow-up times. In this study, multi-center data on patients with known or suspected CAwereas collected from 7 different hospitals and analyzed for all-cause mortality. After adjustment for other risk factors including age, gender, and cardiac risk factors, we found a strong association between an abnormal stress CMR and mortality.
https://jamanetwork.com/journals/jamacardiology/fullarticle/2724474
Detection of ‘silent-MIs’
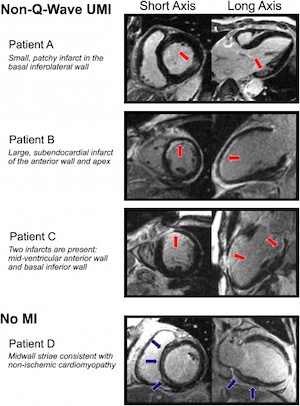
The diagnosis of myocardial infarction is critically important. The label of MI can affect a wide range of issues, including employment, disability claims, insurance, and psychological well-being. Importantly, the diagnosis of MI also impacts clinical management, and the available data indicate that even small infarcts portend worse short- and long-term prognosis. Despite numerous advances in medicine, the diagnosis of MI can still be difficult, as there is marked heterogeneity in the presentation of MI. For example, as many as 1/3 of patients suffer so called ‘silent-MIs’ - infarcts that are associated with minimal or no symptoms. Despite having unremarkable presentations, these infarcts are associated with poor outcomes. Using CMR, we recently evaluated a patient population without a history of MI, but with suspected coronary disease, and found that a significant portion of that population had a previously undiagnosed MI. http://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1000057
Outcomes in non-ischemic heart disease
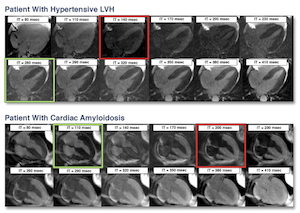
Our research group is actively involved in studies looking at the utility of CMR for diagnosing non-ischemic heart disease and outcomes in these patients. One recent study we conducted evaluated the diagnostic and prognostic utility of a rapid, visual T1 assessment for identification of cardiac amyloid. We found this technique accurately identified patients with myocardial amyloid, and those at increased risk of death. This study suggests strong diagnostic and prognostic utility for this technique in screening patients for cardiac amyloidosis. http://www.sciencedirect.com/science/article/pii/S1936878X13008152
Risk Stratification for Patients Evaluated for Cardiac Defibrillator Implantation
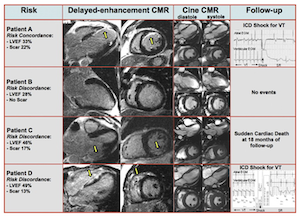
Recent work by our group has evaluated if the assessment of myocardial scarring by CMR could improve risk stratification in patients evaluated for implantable cardioverter-defibrillator implantation. In a patient population undergoing evaluation for possible ICD placement, patients also underwent a CMR exam to identify ejection fraction and scar. We found that myocardial scar as detected by CMR was an independent predictor of adverse outcome in this patient population. http://www.sciencedirect.com/science/article/pii/S0735109712017032
CMR differentiation of acute and chronic MIs
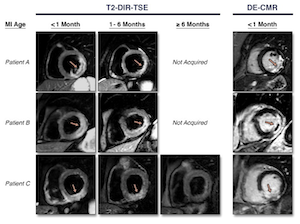
The treatment for an MI depends strongly on the age of the MI. However, it can be difficult to determine infarct age, as an acute MI is often unrecognized, and elevated biomarkers usually resolve after more than a week. Recent work in CMR has focused on using T2-weighted imaging as a method for determining infarct age. Additionally, other CMR markers could provide insight to infarct age, such as the presence of microvascular obstruction, or increased diastolic wall thickness. We compared these techniques in patients with a range of infarct ages. We found T2-weighted imaging was sensitive, but not specific for detection of acute (<1 month old) MIs, while increased diastolic wall thickness and or presence of microvascular obstruction was specific for acute MIs, and the combination of all three methods provided the most precise assessment of infarct age. http://www.sciencedirect.com/science/article/pii/S1936878X15001862